Suspected heart failure
Definition/Description
Clinician has reasonable suspicion of heart failure when the patient has symptoms of recent onset:
- Breathlessness on exertion or at rest
- Orthopnoea or Paroxysmal Nocturnal Dyspnoea ( PND)
- Dependent Oedema in association with other heart failure symptoms
Red Flag Symptoms
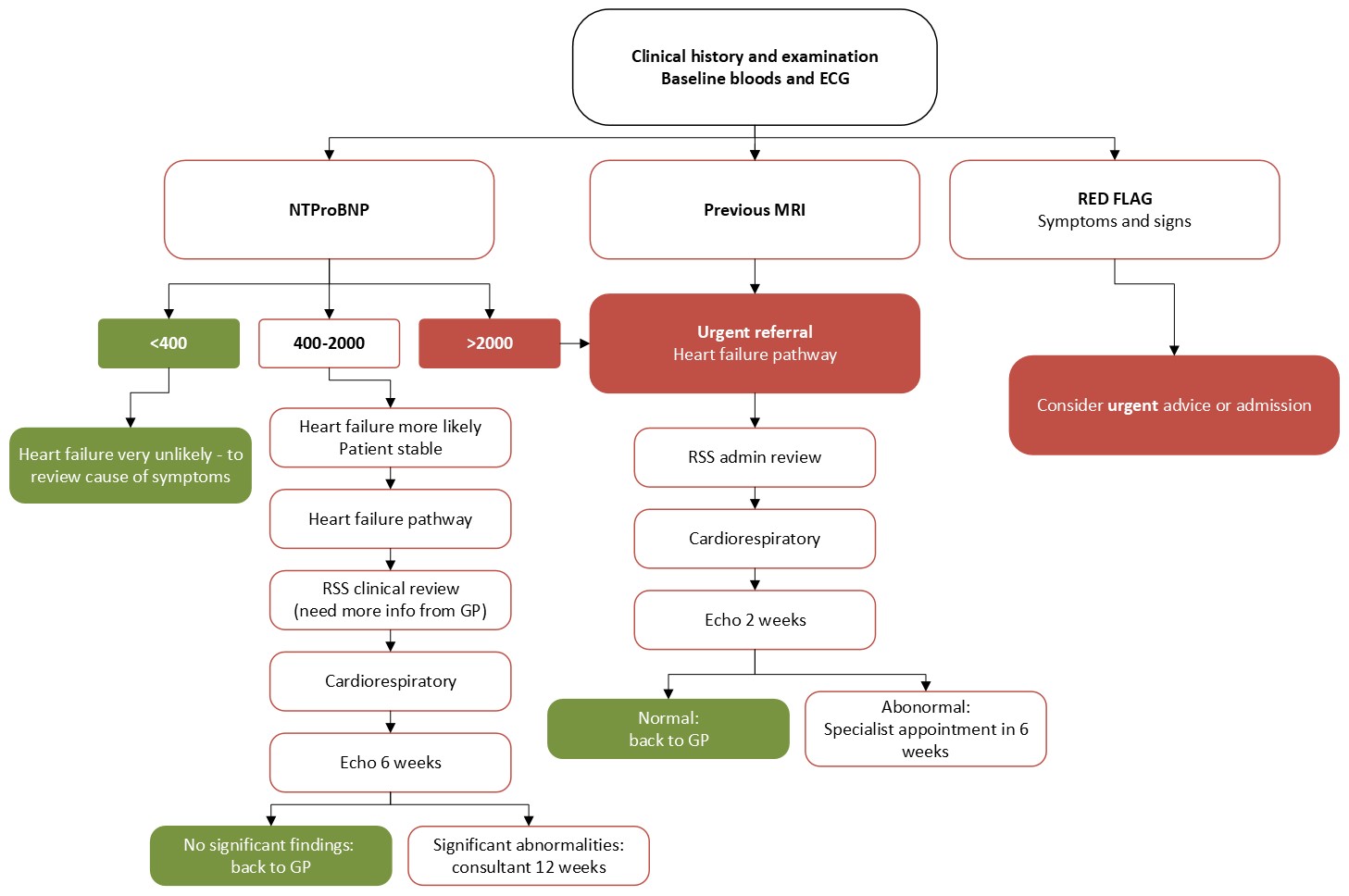
Exclude red flag symptoms and signs where the clinician should consider urgent hospital advice or admission:
- Severe SOB (NYHA III-IV)
- New or escalating PND
- Chest Pain and breathlessness
- Tachycardia > 100 bpm or bradycardia <50bpm
- New onset AF
- Hypoxia <95%
- Syncope or hypotension systolic BP <90 mmHg
- New heart murmur with heart failure symptoms
- Patients with suspected heart failure and a previous MI should be referred urgently to Cardiology ( NICE Quality Standard 1 and 3) via the RSS Heart Failure Pathway (completing all details on the Urgent Proforma and attaching the ECG)
Guidelines on Management
General Points
- The majority of left ventricular systolic dysfunction is caused by ischaemic heart disease
- Other causes for heart failure such as valvular heart disease, or cardiomyopathy should be detected through this pathway
- Clinical history to identify previous cardiac problems (especially MI) and red flag symptoms
- Medications particularly recent changes e.g. rate limiting calcium channel blockers or NSAIDs
- Clinical examination to identify signs of heart failure and red flag signs
New York Heart Association (NYHA) Classifications |
||
Class I |
No limitation of physical activity |
Ordinary physical activity does not cause fatigue, breathlessness or palpitation (includes asymptomatic left ventricular dysfunction) |
Class II |
Slight limitation of physical activity |
Patients are comfortable at rest. Ordinary physical activity results in fatigue, palpitation, breathlessness or angina pectoris (symptomatically ‘mild’ heart failure) |
Class III |
Marked limitation of physical activity |
Although patients are comfortable at rest, less than ordinary activity will lead to symptoms (symptomatically ‘moderate’ heart failure) |
Class IV |
Inability to carry out any physical activity without discomfort |
Symptoms of congestive cardiac failure are present even at rest. Increased discomfort with any physical activity (symptomatically ‘severe’ heart failure) |
Management: Before referral
- ECG to identify previous infarction, abnormal rhythm, (AF, heart block), LBBB and LVH
- Blood tests:- FBC , U & Es, TFTs, LFTs, lipids and glucose/ HbA1c
- CXR to exclude other causes of breathlessness
- If there is a reasonable suspicion of heart failure then BNP should be requested ( NICE Heart Failure Quality Standard 2)
- Medical treatment should be offered with diuretics at this stage to improve symptoms
Outcome AFTER the results are available
- Patients with suspected heart failure and very high levels of NTproBNP > 2000 pg/ml should also be referred urgently via RSS completing the Urgent Proforma as above.
- These high risk patients will all be offered an urgent echo , target within 2 weeks (NICE Quality Standard1) and a specialist assessment arranged ONLY if the echo is abnormal, within 6 weeks.
- If NTproBNP is elevated, 400-2000 pg/ml refer via RSS Heart Failure Service. Patients will be offered an out patient echo. This will be performed within 6 weeks (NICE Quality standard 4 six week assessment and diagnosis)
- Patients identified with significant LVSD (left ventricular systolic dysfunction) will be referred directly to the Cardiology service from echo for specialist assessment and access to the MDT (NICE Quality standard 6). The patient and practice will be notified of the result of the Echo and the plan of action
- Where Echo is normal the patient will be returned to primary care for further tests and consideration of other causes of raised BNP such as AF, ischaemia, right ventricular overload and PE, COPD, CKD, diabetes, age > 70, cirrhosis and heart failure with preserved systolic function (diastolic dysfunction)
- NTproBNP levels of < 400pg/ml in an untreated patient make heart failure unlikely and other causes for breathlessness should be sought particularly anaemia and COPD
- Obesity, diuretics, ACE and ARB, and beta blockers can all reduce levels but are unlikely to normalise levels in a symptomatic patient
BNP testing in Primary Care – repeat testing is rarely needed
NTproBNP testing as part of the Heart Failure Diagnostic and Management Pathway is going well. Although the test is relatively expensive, a level above 400pg/ml identifies those people who are more likely to have significant left ventricular systolic dysfunction (LVSD) and therefore benefit from cardiology input.
Over the past year all of those people with a level > 2000 pg/ml referred through the RSS have been offered an echo appointment within 2 weeks and almost all of those with a level 400-2000pg/ml within 6 weeks.
Overall only 1 in 8 of people with an elevated BNP are shown to have significant Left Ventricular Systolic Dysfunction but 1 in 2 of those with a BNP > 2,000pg/ml have LVSD. It is therefore important to consider other causes of breathlessness particularly in those with only mildly elevated BNP levels.
There are a large number of other factors which raise BNP, such as COPD, CKD and AF for example. The laboratory has recently made the CCG aware of an increase in the number of patients having repeat BNP assessments: with 167 in the past 6 months.
The CCG and lead cardiologist for the heart failure pathway consider that this is only appropriate if the patient is at particularly high risk for heart failure (usually with a significantly abnormal ECG) and has had a recent deterioration in their symptoms and signs. There is no recommendation that repeat BNP should be undertaken for monitoring or surveillance in primary care.
The lab will decline requests for repeat tests within 3 months unless there is detailed information on the request form documenting the deterioration and agreement for testing be sought on a case by case basis.
Referral Criteria/Information
Referrals
- Indications for referral : Recent onset of symptoms and signs of Heart Failure
- Information to include in referral letter : please complete all details on the proforma
- Investigations prior to referral: ECG, FBC, U & E, TFT, LFT, Lipids and glucose/ HbA1c, BNP, CXR
- Referral Criteria PMH MI, or high NTproBNP (> 2000pg/ml) for URGENT referral via RSS
- NTproBNP 400 - 2000pg/ml , no other cause and suitable to refer on the Cardiology, refer via RSS for echo and direct referral on to Cardiology if Echo abnormal
Additional Resources & Reference
Patient information leaflets/ PDAs
- Appropriate information will be given in clinics and by heart failure specialist nurses should the diagnosis be confirmed
GP information
- Heart Failure Provision - Rapid Access Heart Failure Clinic (only available via an N3 connection)
- Community Heart Failure Team (new referral process) (only available via an N3 connection)
- Sacubitril valsartan (Entresto®) - info and checklist for GPs
- Heart Failure MDT template
Referral forms
References
- NICE Chronic Heart Failure Diagnosis Pathway http://pathways.nice.org.uk/pathways/chronic-heart-failure last updated 17 July 2014
- Chronic heart failure: management of chronic heart failure in adults in primary and secondary care. NICE clinical guideline 108 (2010) http://guidance.nice.org.uk/CG108
- NYHA classifications http://www.gpnotebook.co.uk/simplepage.cfm?ID=523567156
Associated Policies
Specialties
Places covered by
- Vale of York
Hospital Trusts
York and Scarborough Teaching Hospitals