Sore throat (acute) in children
Definition/Description
A sore throat is pain or irritation of the throat that often worsens when you swallow. The most common cause of a sore throat (pharyngitis) is a viral infection.
Epiglottitis
Inflammation of structures above the glottis which is usually caused by a bacterial infection. Acute epiglottitis and associated upper airway obstruction has significant morbidity and mortality and is seen as a medical emergency. Haemophilus influenzae type b (Hib) was the most common cause, but Hib vaccine has significantly reduced the rate of epiglottitis. However, other bacterial infection, e.g. Strep pneumoniae, can lead to epiglottitis.
Persisting sore throat
A sore throat lasting for more than three weeks needs a review of their diagnosis, consider noninfectious causes, e.g. gastro-oesophageal reflux or chronic irritation from hayfever
Paediatric Normal Values (adapted from APLS) |
|||
Age |
Resp Rate |
Heart Rate |
Systolic BP |
Neonate <4w |
40-6 |
120-160 |
>60 |
Infant <1 y |
30-40 |
110-160 |
70-90 |
Toddler 1-2 yrs |
25-35 |
100-150 |
75-95 |
2-5 yrs |
25-30 |
95-140 |
85-100 |
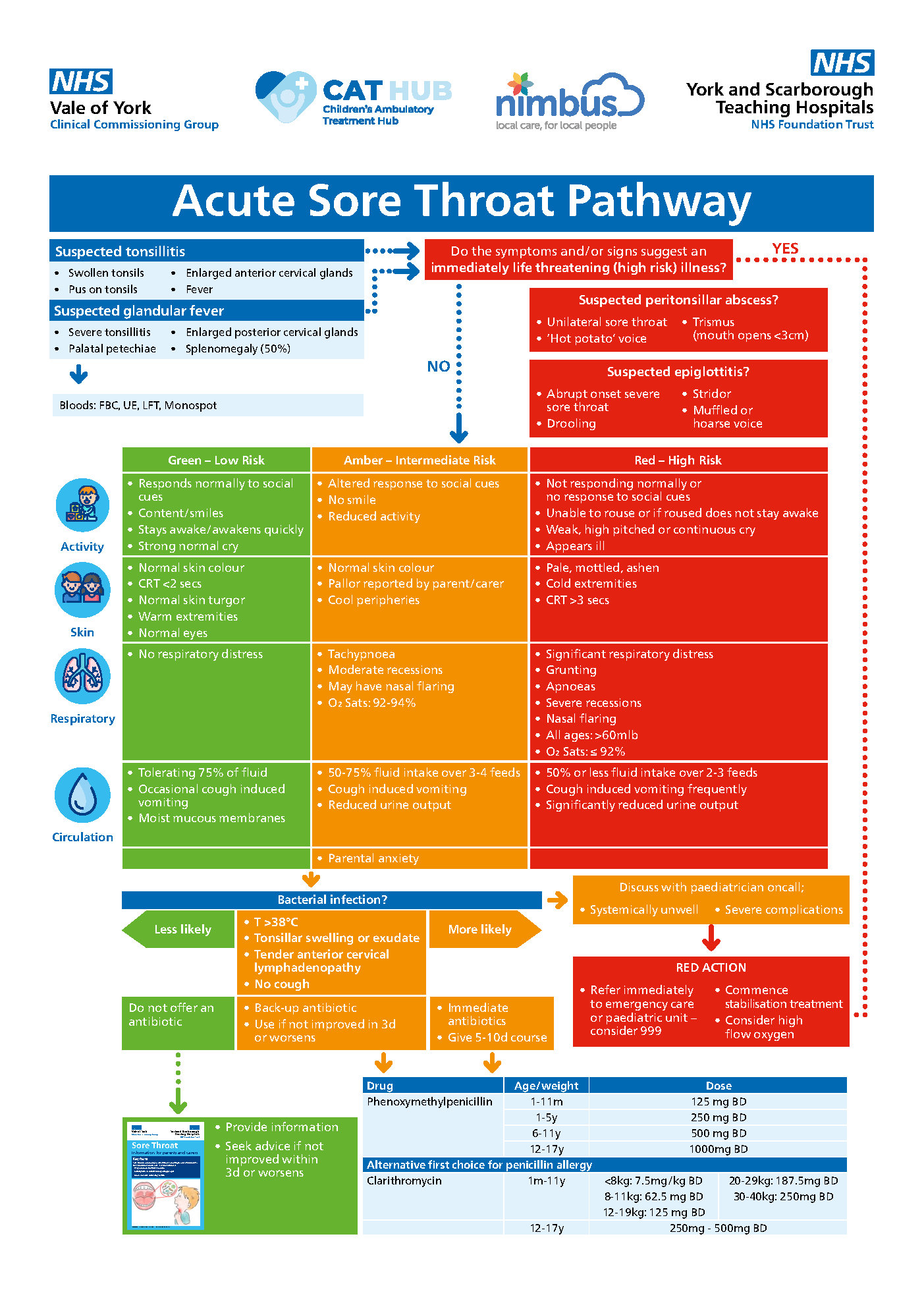
Red Flag Symptoms
Exclude Red Flag Symptoms:
- Epiglottitis; sudden onset of severe sore throat, drooling and systemic signs of infection
- Systemically unwell (red features)
- Stridor or stertor
- Dehydrated
- Swallowing difficulties
- Immunosuppression
Guidelines on Management
General Points
- Rhinovirus, coronavirus, parainfluenza virus are the most common infectious causes (25%)
- Epstein-Barr virus (glandular fever accounts for <1% sore throats)
- Group A beta-haemolytic Streptococcus is the most common bacterial cause of sore throat (15-30% sore throats in children)
- Admission to hospital with severe infection is uncommon and peritonsillar abscesses are very rare in children
- Usually a self-limiting illness with symptoms resolving within three days in 40% and within one week in 85% - irrespective of whether or not the sore throat is due to a streptococcal infection
- Antibiotics may modestly reduce complications and relive symptoms, however there are concerns about resistance.
Differential Diagnoses
Differential Diagnosis |
Clinical Features |
Peritonsillar abscess (rare in children) |
|
Infectious mononucleosis (glandular fever) |
|
Epiglottitis |
If suspected DO NOT EXAMINE THROAT |
Assessment
- Painful swallowing
- Headache
- Fever
- Tender neck due to enlarging lymphadenopathy
To rationalise prescriptions, NICE recommends Centor or FeverPAIN scoring tools to stratify bacterial aetiology in older populations. Centor was created in adult populations 40 years ago. FeverPain was developed in patients aged 3-76 years, with no specific validation in children. Due to the lack of validation of these scoring systems in children it is important to restrict antibiotic use to those who appear clinically unwell, Do not depend on just their score in either of these tools.
Centor criteria (1 point for each) |
FeverPAIN criteria (1 point for each) |
|
Fever |
Fever (during previous 24h) |
|
Tonsillar exudate |
Purulence or pus on the tonsils |
|
Anterior cervical lymphadenopathy |
Attend rapidly (within 3d of onset) |
|
No cough |
Severely inflamed tonsils |
|
No cough or coryza |
Investigations
- Throat swabs should not be carried out routinely; they cannot differentiate between colonisation and infection Suspected infectious mononucleosis
- Bloods: FBC, U&Es, LFTs
- Monospot test:
- Rapid, cheap and specific test that can be performed from the onset of symptoms of infectious mononucleosis
- High sensitivity and specificity in adolescents but are not useful under the age of 4 years
- May be positive in other viral infections, autoimmune disease and haematological malignancies, but do not appear to be positive in primary bacterial infection.
- EBV VCA (viral capsular antigen) IgM and IgG antibody and EBNA IgG
- Preferred over monospot in children under 4 years
- A positive EBV VCA IgM result with negative EBV VCA IgG supports the diagnosis of acute EBV infection
- Enables staging of the infection
Management
- The usual course of antibiotics is about 3 days, but can be up to 1 week
- Oral analgesia
- Consider local analgesics such as benzydamine oromucosal spray, for temporary relief of throat pain. This can be purchased over the counter from pharmacies.
Referral Criteria/Information
When to Arrange Emergency Hospital Admission
- Severe systemic infection
- Suspected peritonsillar abscess
- Suspected epiglottitis
- Immunosuppressed (severe, primarily neutropenic patients or on chemotherapy)
While awaiting admission to hospital
- In suspected epiglottitis
- Allow the child to sit in a comfortable position or on the parent’s lap
- Do not force them to lie down (may precipitate airway obstruction)
- Avoid any examination that will upset the child including examination of the mouth and throat
- Give sufficient supplementary oxygen to try to achieve saturations of at least 92%
Low Risk for Community Management
- No antibiotics: seek advice if symptoms worsen rapidly or significantly, do not improve after 3 days or becomes systemically unwell.
- Delayed antibiotics: start if symptoms do not start to improve within 3 days. Seek medical advice if symptoms worsen rapidly or significantly
- Immediate antibiotics: Give a 5-10-day course.
Community Antibiotic Treatment
- Antibiotics should not be routinely prescribed for acute non-severe sore throat
- Non-severe infection but persistent/worsening symptoms for at least one week
First Line Options |
Age/weight |
Dose |
Phenoxymethylpenicillin |
1-11m |
125 mg BD |
1-5y |
250 mg BD |
|
6-11y |
500 mg BD |
|
12-17y |
1000mg BD |
|
Alternative first choice for penicillin allergy |
||
Clarithromycin |
1m-11y |
<8kg: 7.5mg/kg BD |
8-11kg: 62.5 mg BD |
||
12-19kg: 125 mg BD |
||
20-29kg: 187.5mg BD |
||
30-40kg: 250mg BD |
||
12-17y |
250mg - 500mg BD |
|
Relapsing acute sore throat
- In a child with relapsing infection (e.g. within a six week period) it may be appropriate to take a throat swab sample for culture
- Reasons for relapse may include
- Inappropriate antibiotic therapy
- Inadequate dose or duration of previous therapy
- Patient non-compliance
- Re-infection
- Local breakdown of penicillin by beta-lactamase producing commensals
Referral Information
Indications for referral to ENT The following are indications for consideration of tonsillectomy for recurrent acute sore throat:
- Sore throats are due to acute tonsillitis
- Episodes of sore throat are disabling and prevent normal functioning
- Seven or more well documented, clinically significant, adequately treated sore throats in preceding year
- OR five or more such episodes in each of the preceding two years
- OR three of more such episodes in each of the preceding three years
Additional Resources & Reference
Patient information leaflets/ PDAs
NHS leaflet Colds, coughs and ear infections in children
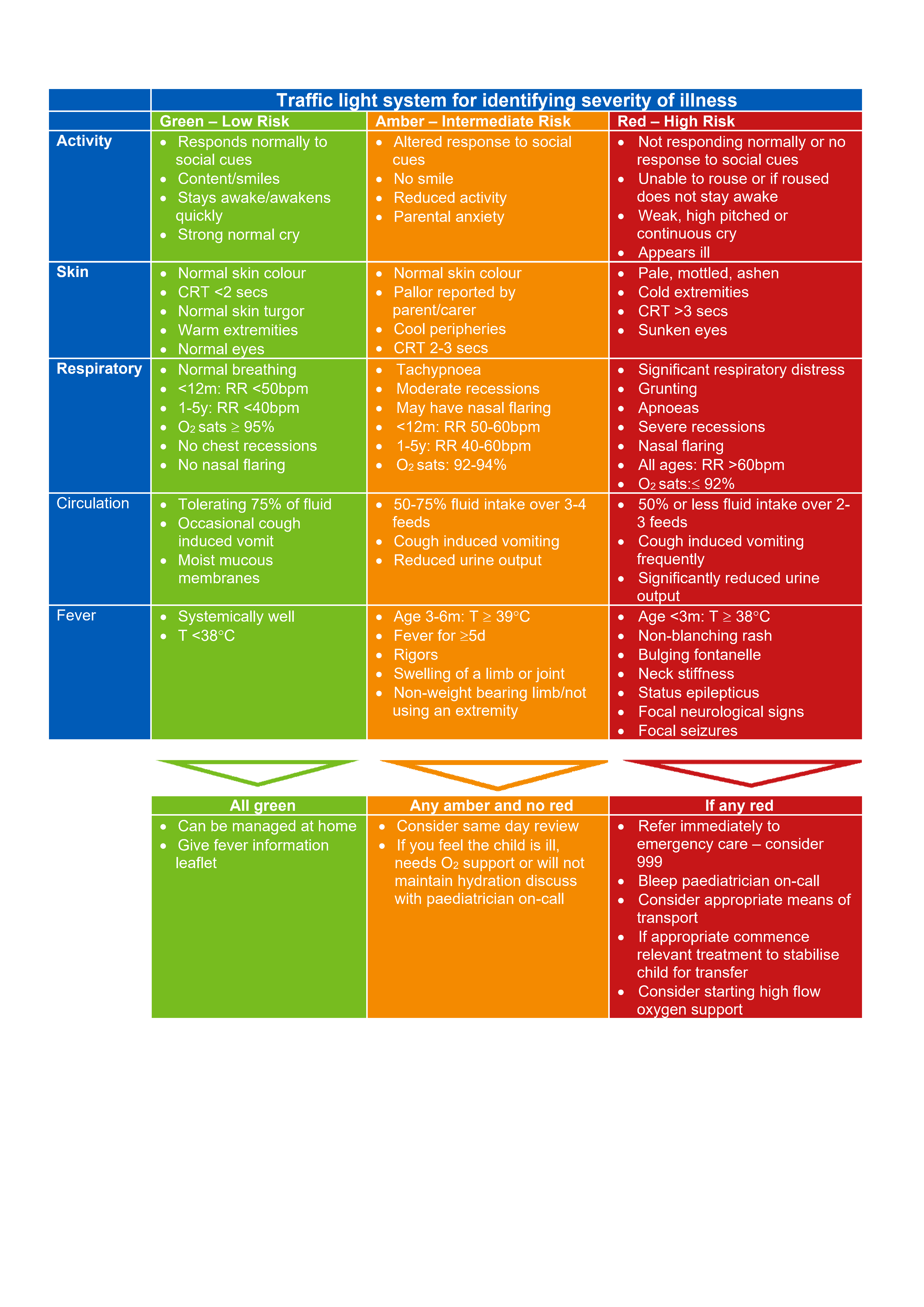
Traffic light system for identifying severity of illness
References
- Arroll B, et al. Are antibiotics indicated as an initial treatment for patients with acute upper respiratory tract infections? A review. N Z Med J. 2008; 121:64-70
- Del Mar CB, et al. Antibiotics for sore throat. Cochrane Database Sys Rev. 2006; CD000023
- NICE. Sore throat (acute): antimicrobial prescribing. (NICE guideline). 2018. National Institute for Health and Clinical Excellence
- Marshall-Andon. How to use…the Monospot and other heterophile antibody tests. Arch Dis Child Educ Pract Ed 2017; 102:188-193 Malley M, et al. Emerg Med J 2021; 0:1-4. doi: 10.1136/emermed-2020-210786
Associated Policies
Places covered by
- Vale of York
Hospital Trusts
York and Scarborough Teaching Hospitals