Gastroenteritis in children (0-5 years old)
Definition/Description
The passage of three or more loose/watery stools per day
Paediatric Normal Values (adapted from APLS) |
|||
Age |
Resp Rate |
Heart Rate |
Systolic BP |
Neonate <4w |
40-6 |
120-160 |
>60 |
Infant <1 y |
30-40 |
110-160 |
70-90 |
Toddler 1-2 yrs |
25-35 |
100-150 |
75-95 |
2-5 yrs |
25-30 |
95-140 |
85-100 |
Red Flag Symptoms
Exclude Red Flag Symptoms (risk of progression to shock)
- Appears to be unwell or deteriorating
- Altered responsiveness (e.g. irritable, lethargic)
- Sunken eyes
- Tachycardia
- Tachypnoea
- Reduced skin turgor
High risk of dehydration
- Children <1 year of age, especially <6 months
- Low birth weight infants
- Vomited ≥ 3 times a day in last 24 hours
- Passing ≥ 6 stools in last 24 hours
- Urinated less than twice in last 24 hours
- Not offered or not tolerated oral supplementary fluids
- Infants who have stopped breastfeeding during illness
- Children with signs of malnutrition
Guidelines on Management
General Points
- The most common cause of diarrhoea in children is acute gastroenteritis
- In children under 5 years around 80% are attributable to viruses
- Rotavirus is the most common cause of medically treated gastroenteritis in resource rich countries, however, since routine Rotavirus immunisation was introduced, the incidence has reduced dramatically
- Dehydration in obese children is frequently under-estimated
- Young infants (<6 months) may progress to shock more rapidly
- Continue or restart the child’s preferred, usual diet as soon as possible, this is particularly important in breastfed children.
Important features in the history
- Onset, sequence and duration of symptoms
- Other family members unwell
- Recent foreign travel
- Consumption of possible unsafe food, e.g. takeaway, BBQ.
- Recent visit to petting farms (E.Coli 0157)
- Recent medication use, particularly antibiotics
- Weight loss
- Known immunodeficiency
Documentation
- Number of episodes of diarrhoea and vomiting in past two to three days.
- Presence of blood in stool.
- Number of times child has urinated in past 24 hours and how many hours since last urine passed
Differential Diagnoses
- Systemic infection, e.g. UTI, pneumonia, sepsis.
- Surgical conditions, e.g. appendicitis, intussusception, sub-acute bowel obstruction.
- Metabolic conditions, e.g. diabetes mellitus.
- Antibiotic associated diarrhoea.
- Haemolytic Uraemic Syndrome. Features that may indicate diagnoses other than gastroenteritis
- Temperature >38C if under 3 months old or >39C if over 3 months old.
- Shortness of breath or tachypnoea.
- Altered level of consciousness.
- Neck stiffness.
- Non-blanching rash.
- Blood and/or mucus in diarrhoea.
- Bilious (green) vomiting.
- Severe or localized abdominal pain.
- Abdominal distension or rebound tenderness.
- Bulging fontanelle (in infants).
Assessment
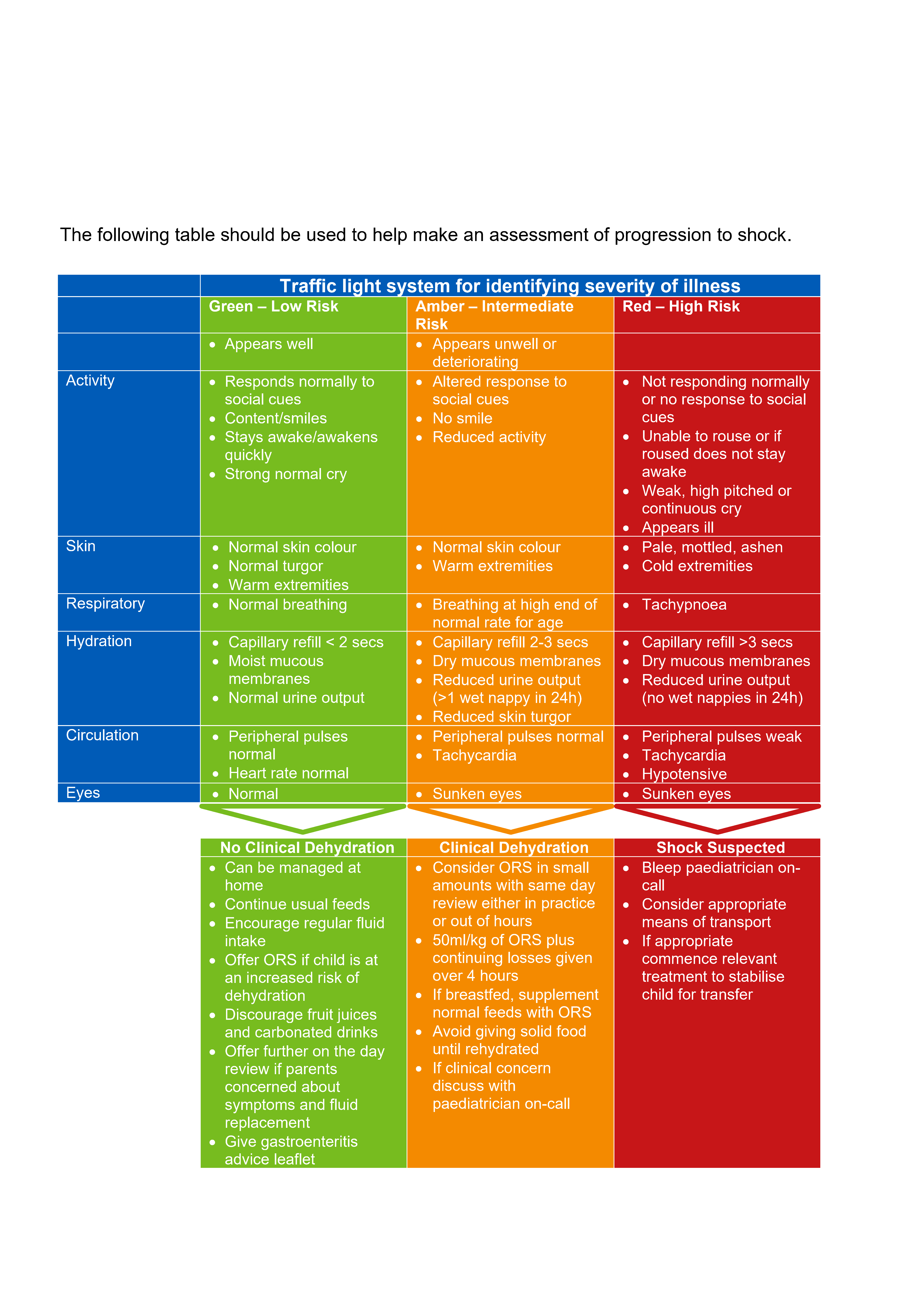
An overall assessment is more accurate than looking at individual symptoms and signs. Prolonged capillary refill time, abnormal skin turgor and absent tears have been shown to be the best individual examination measures to assess for dehydration. (Freedman et al, 2015) See table below
Management in Primary Care
No features of dehydration
- Continue usual feeds.
- Encourage regular fluid intake.
- Offer low-osmolarity oral rehydration salt (ORS) solution if child is at increased risk of dehydration (see maintenance fluid requirements in appendix 1).
- Discourage fruit juices and carbonated drinks.
With features of dehydration but safe to manage at home
- Give ORS solution frequently and in small amounts to rehydrate the child.
- 50ml/kg of ORS plus continuing losses should be given over 4 hours (see fluid deficit in appendix 1).
- If breastfed, supplement normal feeds with ORT.
- If not breastfed, consider supplementing with usual fluids (including milk feeds or water, but not fruit juices or carbonated drinks) if child refuses sufficient quantities of ORS solution.
- Avoid giving solid food until the child is rehydrated.
Seek review if
- Not taking requirements.
- Not keeping fluids down.
- Becoming more unwell.
- Has a reduced urine output.
Medication
- Advise that drug treatment with anti-diarrhoeal drugs, anti-emetics, zinc supplements and probiotics is not recommended for use in children in primary care.
- Do not routinely prescribe antibiotics to children with gastroenteritis
- Arrange treatment of confirmed microbial pathogens, if appropriate, following stool culture and sensitivity testing.
After rehydration
- Restart the child’s preferred, usual diet as soon as possible, this is particularly important in breastfed children.
Stool culture
- Recent foreign travel.
- No improvement in diarrhoea by day 7.
- Recent hospitalisation and/or antibiotic treatment. Reducing cross-infection
- Hand washing.
- Prompt disinfection of contaminated surfaces.
- Prompt washing of soiled clothes.
- Avoid public swimming pools for 2 weeks after diarrhoea has resolved.
Referral Criteria/Information
When to Arrange Emergency Hospital Admission
- Child appears unwell, there are features suggesting severe dehydration and/or progression to shock.
- There is intractable or bilious vomiting.
- There is acute-onset painful, bloody diarrhoea or confirmed E.coli 0157 infection.
- There is a suspected serious complication, e.g. haemolytic uraemic syndrome or sepsis.
When to Consider Hospital Admission
- There are clinical features suggesting a serious alternative diagnosis.
- There is an inadequate response to oral rehydration solution.
- There are red flag features indicting risk of progression to shock.
- There are risk factors for developing dehydration.
Additional Resources & Reference
Patient information leaflets/ PDAs
Patient info/childrens-health/acute-diarrhoea-in-children/gastroenteritis-in-children
Oxfordhealth.nhs.uk - Parent Minor Illness Leaflet
References
- National Institute for Clinical Excellent [NICE] (2009) Diarrhoea and vomiting caused by gastroenteritis in under 5’s: diagnosis and management CG84 [online]
- National Institute for Clinical Excellent [NICE] (2017) Gastroenteritis – Clinical Knowledge Summaries. [Viewed 12 Aug 2021]
- Freedman et al. (2015) Diagnosing clinically significant dehydration in children with acute gastroenteritis using non-invasive methods: a meta-analysis). The Journal of Paediatrics 166(4), 908-916
Appendix 1
Calculation of maintenance fluid requirements The daily fluid requirement can be estimated from the child’s weight using the following formula:
1st 10kg of weight |
100ml/kg |
Per 24h |
2nd 10kg of weight |
50ml/kg |
|
All additional kg of weight above 20kg (up to 50kg) |
20ml/kg |
For example, a 30kg child
First 10kg = 10kg x 100ml/kg = 1000ml
Second 10kg = 10kg x 50ml/kg = 500ml
Additional kg = 10kg x 20ml/kg = 200ml
Total = 1700ml/24h
Calculation of fluid deficit
If dry –give 50ml/kg (5%) for fluid deficit replacement, over 4 hours in addition to maintenance fluid requirements
For example, a 30kg child will require
Deficit = 30kg x 50ml/kg = 1500ml/4h (in addition to maintenance fluid
Trial ORS ml/h according to weight, given in 5-10 min intervals |
|||
Weight (kg) |
Maintenance volume in 24h |
Maintenance fluid every 10 min (ml) assuming 12h non-drinking time in 24h |
Hourly volume (ml) based on 12h non-drinking time |
5 |
500 |
7 |
42 |
6 |
600 |
8.5 |
50 |
7 |
700 |
10 |
59 |
8 |
800 |
11 |
67 |
9 |
900 |
13 |
75 |
10 |
1000 |
14 |
84 |
11 |
1050 |
15 |
88 |
12 |
1100 |
16 |
92 |
13 |
1150 |
16 |
96 |
14 |
1200 |
17 |
100 |
15 |
1250 |
18 |
105 |
16 |
1300 |
18 |
109 |
18 |
1400 |
20 |
117 |
20 |
1500 |
21 |
125 |
25 |
1600 |
23 |
134 |
30 |
1700 |
24 |
142 |
35 |
1800 |
25 |
150 |
40 |
1900 |
26 |
195 |
≥45 |
2000 |
28 |
167 |
Associated Policies
Specialties
Places covered by
- Vale of York
Hospital Trusts
- York and Scarborough Teaching Hospitals