Gastro-oesophageal reflux in children
Definition/Description
Gastro-oeophageal reflux: the passage of gastric contents into the oesophagus. It is a common physiological event that can happen at all ages and is often asymptomatic.
Gastro-oesophageal reflux disease: gastro-oesophageal reflux which leads to symptoms severe enough to merit medical treatments or lead to complications such as oesophagitis or pulmonary aspiration.
Paediatric Normal Values (adapted from APLS) |
|||
Age |
Resp Rate |
Heart Rate |
Systolic BP |
Neonate <4w |
40-6 |
120-160 |
>60 |
Infant <1 y |
30-40 |
110-160 |
70-90 |
Toddler 1-2 yrs |
25-35 |
100-150 |
75-95 |
2-5 yrs |
25-30 |
95-140 |
85-100 |
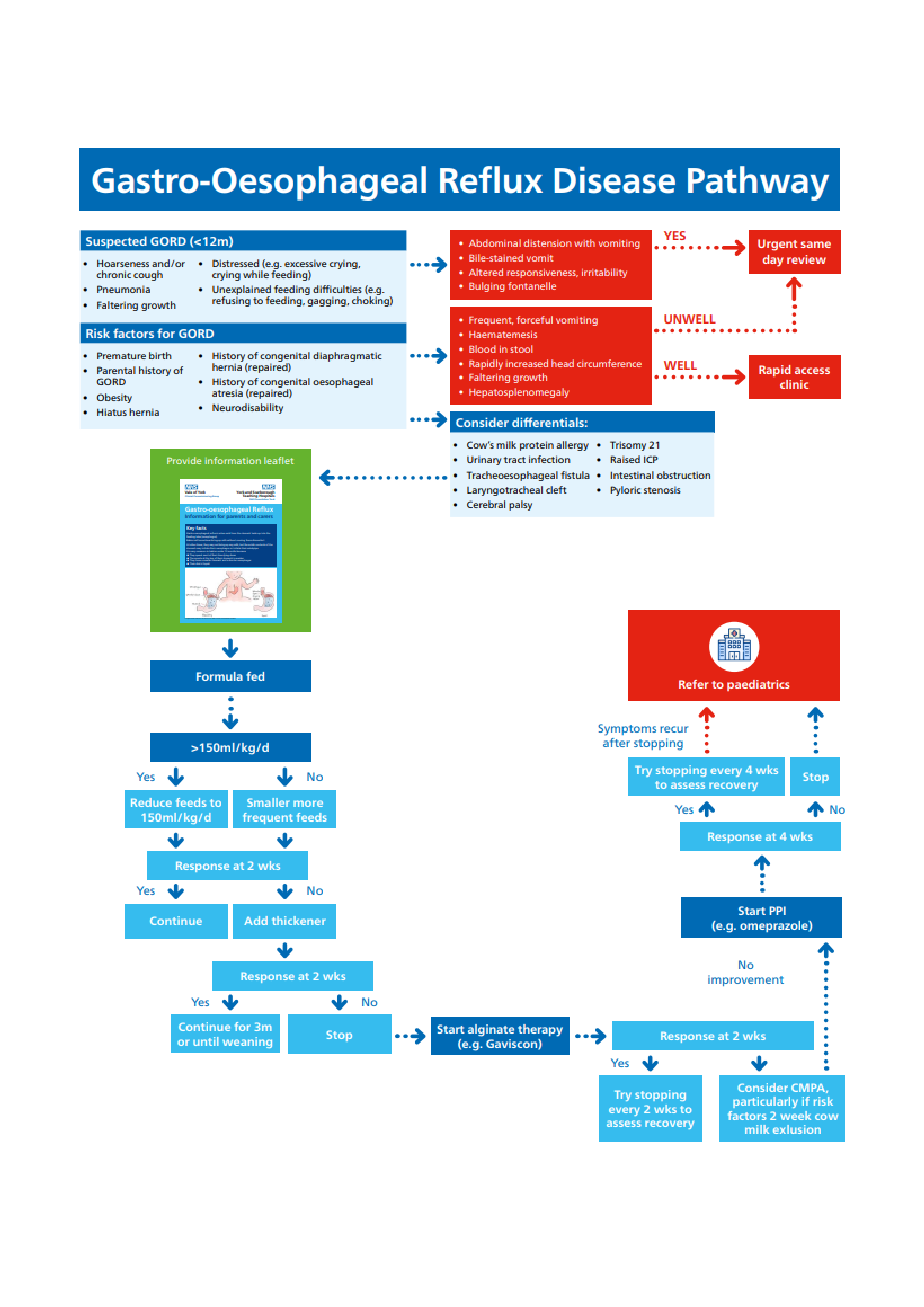
Red Flag Symptoms
Exclude Red Flag Symptoms
- Faltering growth
- Hepatosplenomegaly
Clinical Feature |
Possible diagnosis |
Action |
Abdominal distension, tenderness or palpable mass |
Intestinal obstruction |
Same day |
Bile-stained vomit |
Intestinal obstruction |
URGENT same day |
Frequent, forceful vomiting |
Hypertrophic pyloric stenosis in infants ≤ 2m |
Same day if unwell, or rapid access clinic |
Haematemesis |
Bleed from oesophagus, stomach or upper GI tract |
Same day if unwell, or rapid access clinic |
Blood in stool |
Bacterial gastroenteritis Cows milk protein allergy Acute surgical condition |
Stool for MC&S Same day if unwell, or rapid access clinic |
Chronic diarrhoea |
Cows milk protein allergy |
Assess as per guidelines |
Onset >6m or persisting >1y |
Urinary tract infection |
Urine dip |
Altered responsiveness, irritability |
Illness such as meningitis Safeguarding – occult head injury |
URGENT same day |
Bulging fontanelle |
Raised intracranial, pressure e.g. meningitis |
URGENT same day |
Rapidly increased head circumference, seizures |
Raised intracranial pressure, e.g. hydrocephalus, brain tumour Sandifer syndrome |
Same day if unwell, or rapid access clinic |
Unwell, fever |
May suggest infection |
Assess as per NICE traffic light |
Dysuria |
Urinary tract infection |
Clinical assessment and urine dip |
High risk atopy |
Cows milk protein allergy |
Assess as per guidelines |
Recurrent pneumonia |
Tracheoesophageal fistula |
Same day if unwell, or rapid access clinic |
Aspiration |
Laryngotracheal cleft |
Same day if unwell, or rapid access clinic |
Hypo- or hypertonia |
Cerebral palsy |
Same day if unwell, or rapid access clinic |
Stigmata of genetic disorder |
Trisomy 21 |
Same day if unwell, or rapid access clinic |
High risk of GORD
- Premature birth
- Parental history of GORD
- Obesity
- Hiatus hernia
- History of congenital diaphragmatic hernia (repaired)
- History of congenital oesophageal atresia (repaired)
- Neurodisability
Guidelines on Management
General Points
- Affects 40% of infants
- Usually begins before the infant is 8 weeks old
- Transient lower oesophageal sphincter relaxations have been shown to be the predominant mechanism of reflux
- Signs and symptoms of possible regurgitation, reflux and colic are rarely associated with any underlying pathology in infants who are gaining weight and developing normally.
- Only a small proportion will need to be clinically managed as GORD
- Symptoms in infants typically resolve without treatment (resolves in 90% by 1 year)
Differential Diagnoses
- Safeguarding – persistent irritability and vomiting may be a sign of occult head injury. You must document head circumference every time you see an infant
- Intestinal obstruction – bile-stained vomit
- Hypertophic pyloric stenosis – frequent, forceful vomiting
Investigations
Usually investigations aren’t indicated for GOR, therefore most children will not require any investigations.
Management
Key principles
- Do NOT recommend positional management to treat GOR in sleeping infants. Infants should be placed on their back when sleeping.
- Keep baby upright for as long as possible after feeds
- Baby-wearing (use of slings/carriers)
- Avoid tobacco smoke exposure
- Encourage breastfeeding
Formula Fed Infants
- Formula fed, check for overfeeding: normal volume of feed in 100-150ml/kg/d
- If excessive, reduce feed volumes for infants weight (>150ml/kg/d)
- If normal feed volume, suggest smaller volume, more frequent feeds (6-7 feeds/24h)
Thickened Formula
- Thickened formulae reacts with stomach acid, thickening in the stomach rather than the bottle so there is no need for a fast-flow teat.
- Thickened formula needs to be prepared with cooled pre-boiled water, which is against recommendation of using boiled water to make the milk which is then cooled to 70C
- Consider trial of thickened formula for 2 weeks
- If no improvement after 2 weeks stop
- If improvement continue for 3m or until weaning
Carobel: first line option to thicken feeds. It enables easy reassessment of ongoing need as it can easily be omitted from periodic feeds.
- Add ½ scoop to 90ml cooled boiled water (still warm). Shake well and leave to thickened for 3-4 minutes
- Shake again and feed • Thickness can be increased using 1 scoop in 60ml
- These thicken in the bottle, so need to be given with a fast-flow teat
- Do not prescribe Gaviscon concurrently with a thickening agent
Evidence of benefit for thickeners is mixed. They may delay gastric emptying.
Breast Fed Infants
- Skilled breastfeeding assessment
- Breastfeeding should not be stopped for the purposes of thickening feeds
Medication
- Evidence suggests acid-suppressing medications are not effective in infants for treatment of symptoms such as regurgitation and irritability
- NICE gives some recommendations for prescribing Gaviscon if conservative measures have failed Infant Gaviscon: 1 dual sachet = 2 doses
Infant Gaviscon: 1 dual sachet = 2 doses
<4.5kg: 1 dose when required up to a maximum of 6 times in 24 hours
>4.5kg: 2 doses when required up to a maximum of 6 times in 24 hours
Bottle fed: Mix in 115ml (4oz) of feed
Breast fed: Mix into cooled boiled water or expressed breastmilk and give with a spoon
N.B. prescribed with directions in terms of ‘dose’ to avoid errors. Many notice their baby’s stool becomes firmer.
If no improvement after 2 weeks, consider Cow’s milk protein allergy (CMPA) or refer to paediatrician
If improvement after 2 weeks, try stopping at regular intervals for recovery assessment
Safety Netting
Advise parents they should return for review if any of the following occur
- Regurgitation becomes persistently projectile
- Bile-staining vomiting (green)
- Haematemesis (blood in vomit)
- New concerns such as marked distress, feeding difficulties or faltering growth
- Persistent, frequent regurgitation beyond the first year of life
Referral Criteria/Information
Indications for referral
- No improvement in regurgitation >1y
- Persistent faltering growth secondary to regurgitation, feeding aversion and regurgitation
- Suspected recurrent aspiration pneumonia
- Frequent otitis media
- Suspected Sandifer syndrome
- Unexplained apnoea
Additional Resources & Reference
Patient information leaflets/ PDAs
References
- D D, E S-B, A L, et al. Effects of Smoking Exposure in Infants on Gastroesophageal Reflux as a Function of the Sleep-Wakefulness State. J Pediatr 2018;201:147–53. doi:10.1016/J.JPEDS.2018.05.057
- HJ H, HE J, JL B, et al. Influence of breast versus formula milk on physiological gastroesophageal reflux in healthy, newborn infants. J Pediatr Gastroenterol Nutr 1992;14:41–6. doi:10.1097/00005176-199201000- 00009
- R R, Y V, M S, et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutritio. J Pediatr Gastroenterol Nutr 2018;66:516–54. doi:10.1097/MPG.0000000000001889
- SR O, E H, W F-J, et al. Multicenter, double-blind, randomized, placebo-controlled trial assessing the efficacy and safety of proton pump inhibitor lansoprazole in infants with symptoms of gastroesophageal reflux disease. J Pediatr 2009;154. doi:10.1016/J.JPEDS.2008.09.054
- H W, P K-N, SH M, et al. Efficacy and safety of pantoprazole delayed-release granules for oral suspension in a placebo-controlled treatment-withdrawal study in infants 1-11 months old with symptomatic GERD. J Pediatr Gastroenterol Nutr 2010;50:609–18. doi:10.1097/MPG.0B013E3181C2BF41
- RJ van der P, MJ S, MP van W, et al. Efficacy of proton-pump inhibitors in children with gastroesophageal reflux disease: a systematic review. Pediatrics 2011;127:925–35. doi:10.1542/PEDS.2010-2719
- M T, NA A, A B, et al. Pharmacological treatment of children with gastro-oesophageal reflux. Cochrane database Syst Rev 2014;2014. doi:10.1002/14651858.CD008550.PUB2
- Scenario: Management | Management | GORD in children | CKS | NICE. https://cks.nice.org.uk/topics/gord-in-children/management/management/ (accessed 7 Jul 2021).
- Tulleken C van. Overdiagnosis and industry influence: how cow’s milk protein allergy is extending the reach of infant formula manufacturers. BMJ 2018;363. doi:10.1136/BMJ.K5056
- M G, E B, M S, et al. Dietary modifications for infantile colic. Cochrane database Syst Rev 2018;10. doi:10.1002/14651858.CD011029.PUB2
Associated Policies
Places covered by
- Vale of York
Hospital Trusts
York and Scarborough Teaching Hospitals