Post-menopausal bleeding
Definition/Description
- PMB is defined as a single episode of vaginal bleeding after the age of 55, occurring 12 months or more after the last period. It is associated with a 10% risk of malignancy.
- Under age 55, a single episode of light bleeding or bleeding of a menstrual nature (5-7days) does not routinely need any further investigations.
- Consider USS if risk factors are present:
- Obesity
- Type 2 diabetes
- Family history of endometrial cancer
- PCOS
- Heavy or recurrent episodes of bleeding
- Consider USS if risk factors are present:
Red Flag Symptoms
- Cervical tumour should be excluded by speculum examination (refer 2WW pathway)
- Urological Cancer should be considered- Urinalysis performed if no vaginal bleeding seen on examination. (follow Haematuria pathway)
Guidelines on Management
- All women presenting with PMB require a vaginal examination and Speculum examination.
- Urinalysis should be performed if no vaginal bleeding seen.
- Women on tamoxifen or those with recurrent bleeding within 6 months of a normal scan and possible causes such as atrophy treated should be referred straight to 2WW pathway.
- Refer for FAST-TRACK USS clearly stating “PMB”.
- Postmenopausal women on HRT with abnormal bleeding should be advised to stop for 6 weeks and if problem continues, then treat as PMB (fast-track USS first line).
- Reminder: USS is unreliable method for assessing endometrium if a coil is in situ. Usually appropriate to remove the coil and organize an USS if problem persists. If unsure about coil removal please use A&G to seek advice from gynaecology team
USS Results are sent back to GP for action
- If normal (ET ≤ 4mm), then manage any underlying cause e.g. atrophic vaginitis.
- If scan suspicious - then the Gynaecology 2WW form should be completed and the patient will be offered direct access Outpatient Hysteroscopy.
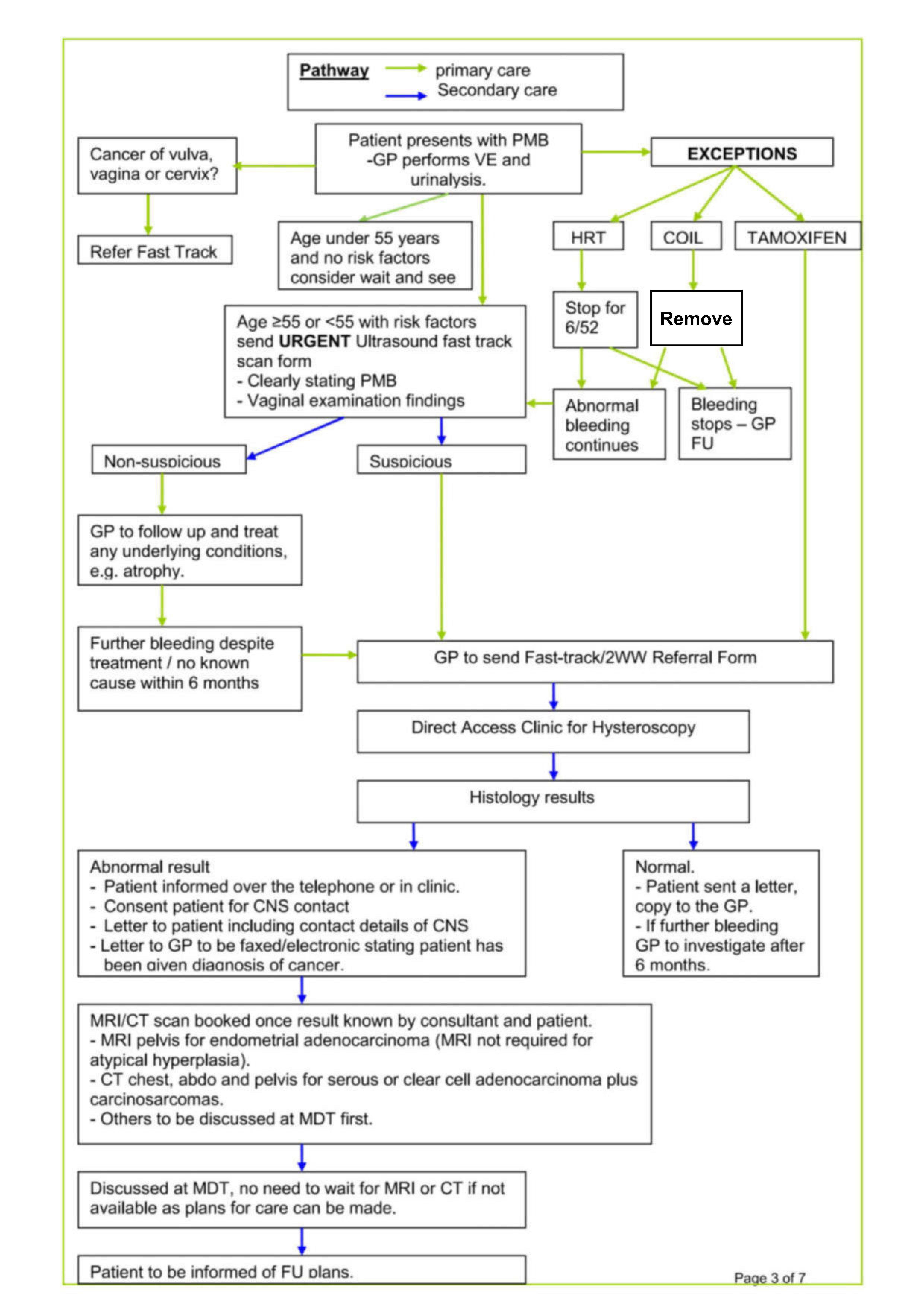
See PMB pathway flowchart below for more detailed management in specific circumstances
Referral Criteria/Information
Investigations prior to referral
- USS: for all low risk patients
- Urinalysis (if no cause for bleeding seen)
- Fast-track Form for all High Risk patients and patients with abnormal USS
- BMI
- Complex medical situations (e.g. multiple co-morbidities/severe mobility restrictions) can be discussed directly with Miss Claire Oxby or another gynaecology consultant.
Additional Resources & Reference
Patient information leaflets/ PDAs
References
- Management of Women with Postmenopausal Bleeding guidance Version No. 4, March 2018 – October 2020
- NICE 2015: suspected cancer guidelines
Associated Policies
There are no associated policies.
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals
Date created: 13/08/2025, 10:51
Last modified: 13/08/2025, 11:01
Date of review: 2024. 09. 30.