Bone protection service
Definition/Description
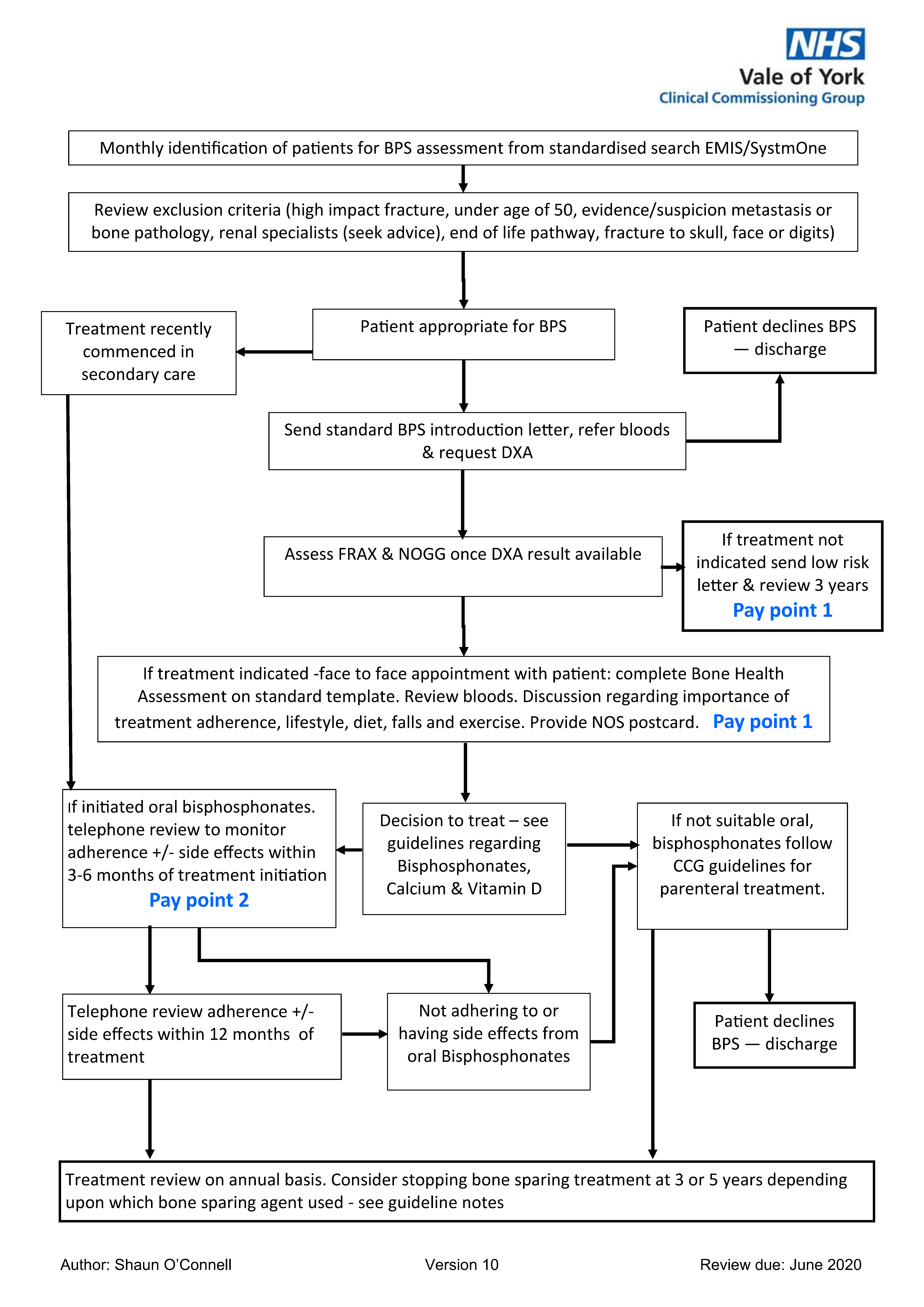
The service aims to identify patients who have had a bone fracture and reduce their risk of subsequent fractures.
Exclusion Criteria:
- Under the age of 50;
- fracture due to high trauma;
- fracture of the skull, nose, digits, facial bones;
- patient on the end of life pathway;
- evidence or suspicion of metastasis or other bone pathology;
- patient known to have a significant renal impairment with eGFR <35 and/or is known to the renal team
Red Flag Symptoms
None provided
Guidelines on Management
DXA:
A DXA scan should be requested in all patients who are able to attend for investigation. In practical terms this means being able to get up on to the scanner couch and then being able to lie flat for a few minutes whilst images are taken. A hoist is available if required and this must be highlighted on the referral. Axial DXA followed by use of FRAX (ideally within 12 weeks of fracture) will indicate whether prescribing of bone sparing agent is appropriate and it will provide a baseline measurement for evaluation of response to treatment.
The Vale of York CCG feeIs it is reasonable to consider a DXA scan in patients over 75 years, where life expectancy exceeds the 3-5 years needed to gain benefit from Osteoporosis treatment.
The presence of vertebral fractures indicates a greater risk of future fractures and may influence the choice of treatment for an individual, IVA (Inter-vertebral Analysis) can be carried out with DXA.
If bone sparing treatment is not indicated at initial assessment, reassess as per initial assessment after 3 years. Consider need for a new DXA scan and new FRAX calculation.
Bloods:
Relevant laboratory tests can unmask any potential secondary causes of osteoporosis and inform treatment decisions (NOS Quality standards for Osteoporosis and prevention of fragility fractures, 2017). Consider non-osteoporotic causes such as:
- metastatic bone cancer,
- multiple myeloma,
- osteomalacia,
- Paget’s disease,
- premature menopause,
- hypogonadism in men,
- diabetes,
- hyperthyroidism,
- inflammatory arthropathies,
- chronic gastrointestinal disease such as inflammatory bowel disease, coeliac disease or malabsorption,
- chronic liver disease
- conditions that require long term steroid use e.g. COPD, polymyalgia rheumatica
Relevant blood tests - depending on clinical circumstances:
- Full blood cell count
- HbA1c
- Renal Function
- C-reactive protein
- Serum calcium, albumin, phosphate, alkaline phosphatase and liver transaminases
- Thyroid function tests
Other tests which may be indicated – depending on clinical circumstances:
- Serum protein immunoelectrophoresis and urinary Bence-Jones protein
- Serum 25-hydroxyvitamin D Plasma parathyroid hormone
- Serum testosterone (men), sex hormone binding globulin, folliclestimulating hormone (women), luteinizing hormone (women)
- Serum prolactin
- 24-hour urinary free cortisol/overnight dexamethasone suppression test
- Isotope bone scan
Diet and Lifestyle – NOS publications
Discussion regarding dietary calcium – Use calcium calculators
- Use IOF Calcium calculator for patients who are dairy intolerant / non-dairy lifestyle
- Smoking cessation
- Reduce alcohol especially if intake if >3 units per day
- Regular weight bearing exercise, if appropriate
- Suggest contacting National Osteoporosis Society (NOS) and provide patient with NOS postcard. The NOS helpline can also be used by patients and clinicians (Free call - 0808 800 0035). Practices should order their free copies of the postcard
Treatment with medication:
When the patient has had a DXA, calculate the FRAX and press the ‘View NOGG Guidance’ button to determine the need for bone sparing treatment:
If bone sparing treatment is not indicated provide with diet and lifestyle leaflet low risk patient information and reassess as per initial assessment after 3 years. Consider need for a new DXA scan and new FRAX calculation
Calcium and/or Vitamin D supplements:
Calcium & Vitamin D Medal ranking
The Department of Health recommends Vitamin D for all people aged over 65. Follow CCG guidelines on specific drugs and follow GMC guidance that you must make good use of the resources available to you (Good Medical Practice 2013).
If at High Risk of Future Fracture recommend Bone Sparing Treatment:
Unless contraindicated start Alendronic acid 70mg weekly. Provide patients with How to take your bisphosphonate tablets and the patient information leaflet for Alendronic acid
There are alternatives Bisphosphonates and other drugs affecting bone metabolism if patients are unable to take Alendronic acid each week or are intolerant.
FOR ALL BISPHOSPHONATES. All patients should have a dental check-up (and any necessary remedial work should be performed) before bisphosphonate treatment, or as soon as possible after starting treatment. Patients should also maintain good oral hygiene, receive routine dental check-ups, and report any oral symptoms such as dental mobility, pain, or swelling, non-healing sores or discharge to a doctor and dentist during treatment.
https://bnf.nice.org.uk/drug/alendronic-acid.html
https://www.gov.uk/drug-safety-update/bisphosphonates-osteonecrosis-of-the-jaw
At the time of writing, Vale of York CCG is expecting to commission a primary care service for the administration of parenteral alternatives.
HRT is recommended by NICE CKS for women who have experienced a premature menopause until the age of 50. NOS recommend it for women under the age of 60 years when the benefits of treatments outweigh the risks [National Osteoporosis Society, 2010]. NICE CKS considers this to be the case when non-oestrogen treatments are unsuitable and there is a significant risk of a fragility fracture. Patients should be made aware of the risks and benefits of HRT.
Follow up: (Can be done by telephone by Pharmacist or practice nurse)
Set review date for 3-6 months and at 12 months from medication start date to review adherence and tolerance of medication. You should ask the patient how they are taking the medication, including day of week they choose, what drink they take it with and do they forget it; to correct any habits that will result in the medication not having optimal effect.
Also consider falls risks at subsequent review appointments.
Review at 3-5 years:
NICE guideline (NG56) 2016 on Multimorbidity states in para 1.6.16 that [clinicians should]:
Tell a person who has been taking bisphosphonate for osteoporosis for at least 3 years that there is no consistent evidence of:
- further benefit from continuing bisphosphonate for another 3 years
- harms from stopping bisphosphonate after 3 years of treatment. Discuss stopping bisphosphonate after 3 years and include patient choice, fracture risk and life expectancy in the discussion.
The NOS guidance recommends treatment with bisphosphonates beyond five years though NICE’s current position is not clear.
The NICE quality standard (QS 149, 2017) states: The optimal duration of bisphosphonate therapy is unclear and there are possible adverse effects of longterm treatment. A medication review for people having long-term bisphosphonate therapy gives the opportunity to consider whether continuing treatment is the best option, or if treatment should be changed or stopped. The response to treatment may also be evaluated to help determine whether to continue treatment.
The NICE accredited NOGG guidelines 2017 state:
Continuation of treatment is recommended for people with any of the following risk factors:
- age over 75 years
- previous hip or vertebral fracture
- one or more low trauma fractures during treatment (after poor adherence to treatment, for example less than 80% of treatment has been taken, and causes of secondary osteoporosis have been excluded)
- current treatment with oral glucocorticoids of 7.5 mg or more prednisolone/day or equivalent.
For people without risk factors, arrange a dual-energy X-ray absorptiometry (DXA) scan and consider:
- Continuing treatment if the T-score is less than -2.5, and reassessing fracture risk and bone mineral density (BMD) every 3 to 5 years.
- Stopping treatment if the T-score is greater than -2.5, and reassessing their fracture risk and BMD after 2 years.
There is no evidence base to guide decisions about treatment beyond 10 years and management of such patients should be considered on an individual basis.
If a fracture is sustained whilst on treatment:
Advice and guidance locally is from the secondary care Elderly Medicine Consultant. Consider the need for secondary screening of osteoporosis bloods: FBC, CRP, U&E’s, Liver Function Tests and Calcium, Thyroid Function Tests, Serum Protein Electrophoresis, Parathyroid hormone, Coeliac screen, Vitamin D status, 9am testosterone level in males >65 years.
Sustaining a second fragility fracture should precipitate re-entry into bone protection service pathway to ensure all appropriate investigations are completed and to ensure continuing bone health treatment is optimal.
Referral Criteria/Information
Patients should be invited to attend the bone protection service by letter patient introduction letter and offered a DXA scan (NICE says offer a dual-energy X-ray absorptiometry DXA) to measure bone mineral density (BMD).
If the patient is unable to tolerate the primary care treatment options, please seek advice from secondary care Elderly medicine consultant. If unsure, a referral to Elderly medicine clinic is appropriate.
Assessment of falls risk:
In most cases, a fragility fracture will result from a fall. A history of falls in the past year is the single most important risk factor for falls.
Patients should be asked whether they have fallen in the last 12 months. Observe gait and balance and complete falls risk assessment tool.
For patients with a more complex history of falls there is an Elderly medicine falls clinic at St Helens, into which GPs can refer via RSS. This clinic requires the patient to attend for a full morning assessment as they are seen by the multidisciplinary team- Consultant, Nurse, Physio/OT and for observations and bloods and if appropriate referred to their falls and balance exercise group.
Locality specific Physiotherapy/OT adopt a ‘falls are everyone’s business’ approach Community Therapy Services
Additional Resources & Reference
For local authorities exercise programmes and referrals see Community Services page
Additional information
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals