Suspected liver disease / deranged LFTs
Definition/Description
This guidance covers:
- Steatotic Liver Disease (formally fatty liver disease)
- Alcohol-related liver disease
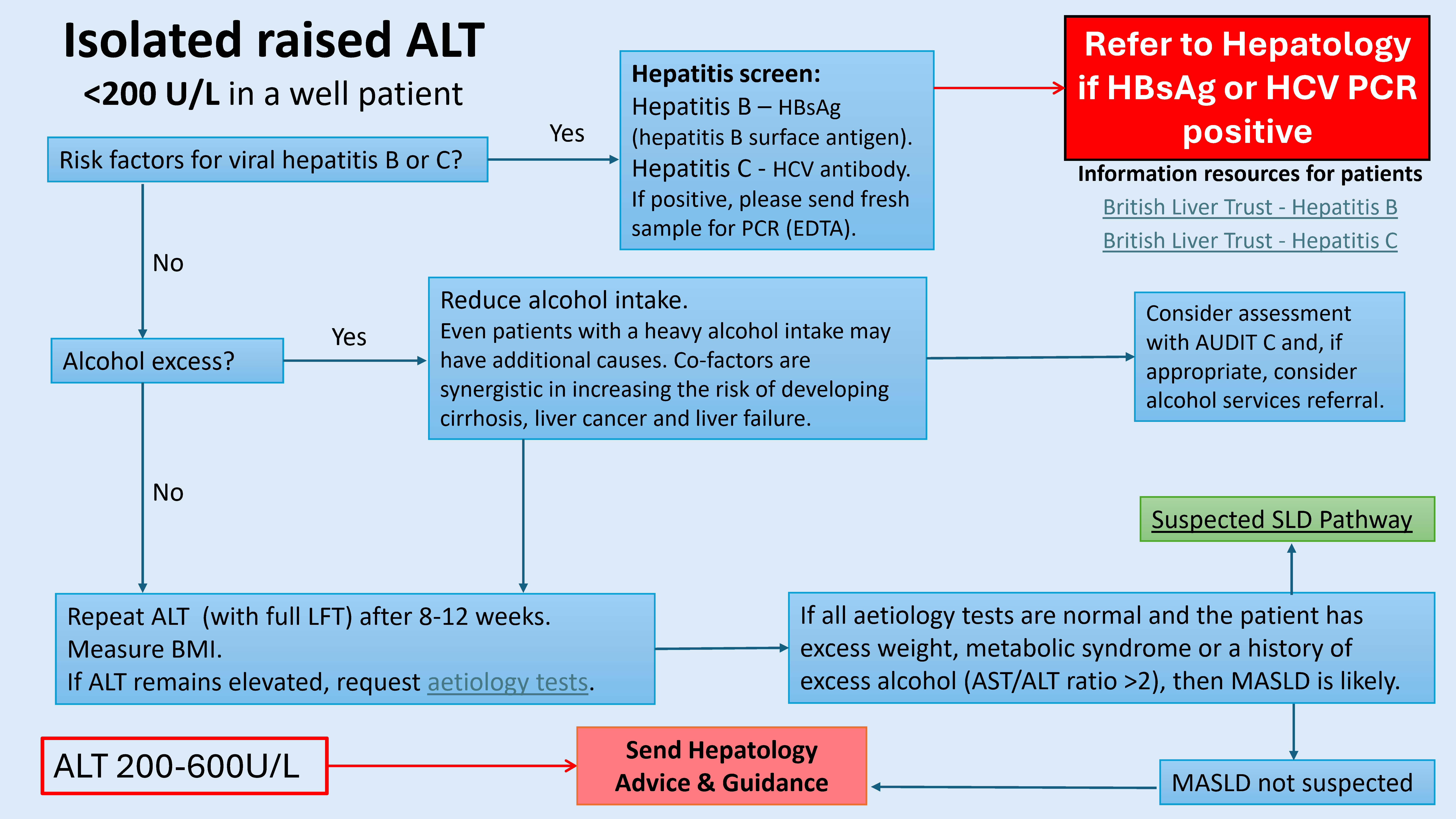
- Isolated raised ALT <200 U/L
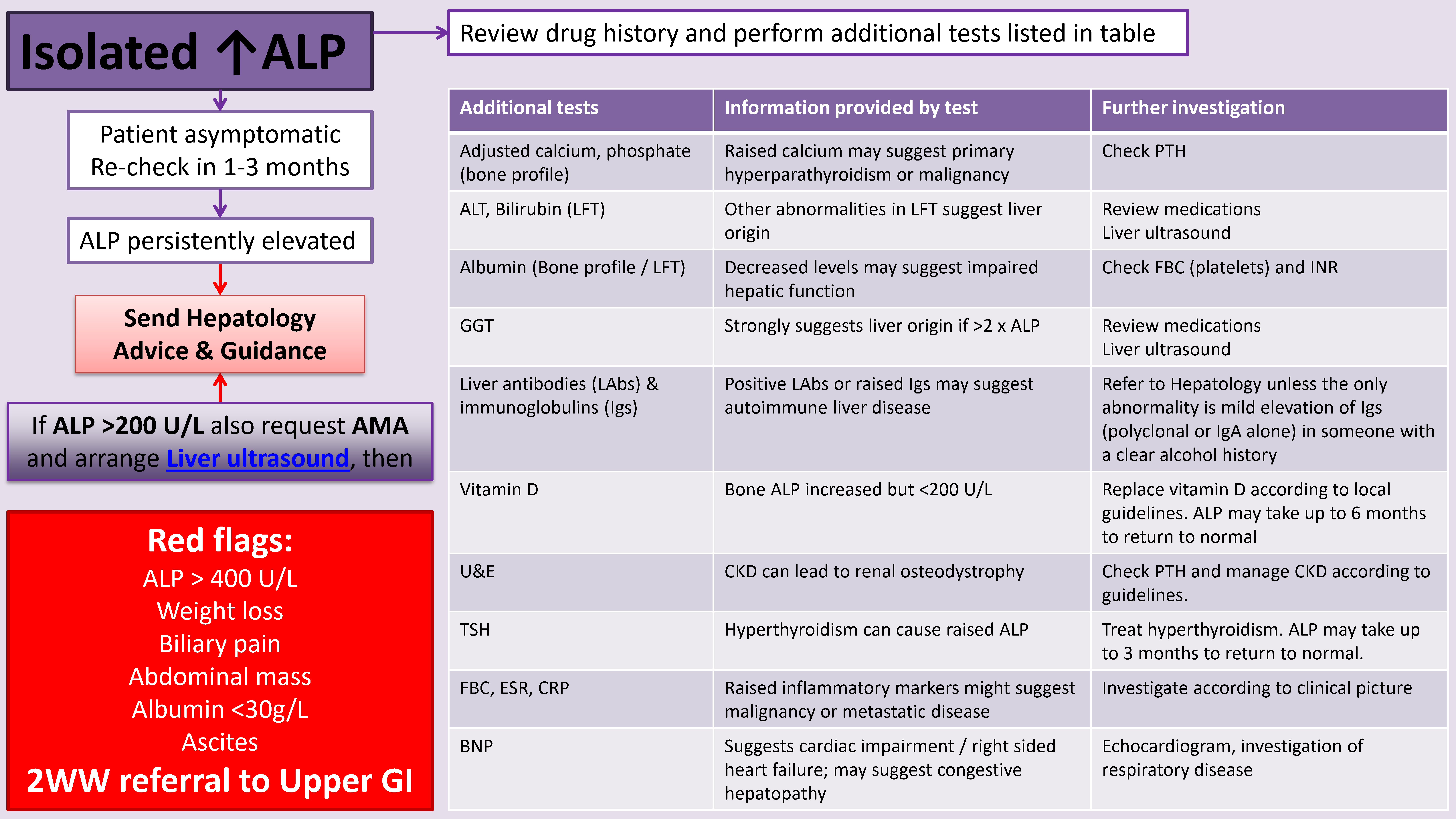
- Isolated raised ALP <1000 U/L
- Isolated raised bilirubin
This guidance is most applicable to the “well” person with possible of chronic liver disease, or the patient with an incidental finding of raised liver enzymes.
There has been a marked rise in deaths from liver disease in England over the last 10 years. The majority of chronic liver disease can be prevented or treated with early diagnosis or intervention, but disease is typically very advanced before symptoms present. At this stage, there is little chance of preventative or curative treatment.
The Yorkshire and Humber Liver Network recommend investigation of all abnormalities in LFTs, in order to
a. seek an explanation and diagnosis
b. seek a diagnosis for which preventative measures may reduce risk of progression to liver failure and premature death
c. seek a diagnosis for which specific treatment can reduce risk of progression to liver failure, liver cancer and premature death.
Consider screening for abnormal liver blood tests or Steatotic Liver Disease (SLD) in patients with:
- type 2 diabetes mellitus
- obesity
- hypertension
- hypercholesterolaemia
- harmful alcohol consumption
Red Flag Symptoms
Emergency admission (risk of acute liver failure):
- ALT > 600U/L with prolonged INR / PT or symptoms of confusion
Contact Gastro Reg (or Med Reg out of hours) via Hospital switchboard:
- ALP >1000 and / or ALT >600 and / or jaundice with ANY elevation in ALP or ALT
Patients with acute hepatitis often present unwell/ symptomatically and/or have very high transaminases.
Urgent Hepatology Referral:
Request aetiology investigations, state that acute hepatitis is suspected AND request
- URGENT viral serology, including Hepatitis A, B, C and E
- CMV and EBV (and HSV if any history or signs of cold sores etc)
If there is any history of intravenous drug use in the previous 12 weeks hepatitis C PCR should be specifically requested (HepC antibody may be negative).
Guidelines on Management
History
- Ethnic background
- Recent travel history
- Exposure to people with jaundice
- Exposure to potentially contaminated foods
- Occupational exposure to hepatotoxins
- Alcohol consumption (with a view on hazardous or harmful drinking)
- Family history
- Features of metabolic syndrome:
- diabetes
- Increased BMI or WHR
- hypertension
- hypercholesterolaemia
- hyperuricaemia
- Risk factors for metabolic dysfunction-associated steatotic liver disease (MASLD):
- social deprivation
- age older than 50 years
- metabolic syndrome
- Possible parenteral exposures:
- Blood transfusions
- intravenous (IV) or intranasal drug use (at any time)
- tattoos
- sexual activity
Examination
- Examine for:
- jaundice
- stigmata of chronic liver disease:
- spider naevi
- palmar erythema
- gynaecomastia
- flapping tremor
- palpable liver or spleen
- ascites
- Measure BMI
- Features of chronic liver disease:
- spider naevi,
- palmar erythema
- hepatomegaly
- splenomegaly
- ascites
- Prodromal viral symptoms:
- jaundice
- arthralgias
- myalgias
- rash
- anorexia
- weight loss
- pain, fever, and rigors
- pale stools, dark urine
- skin itching
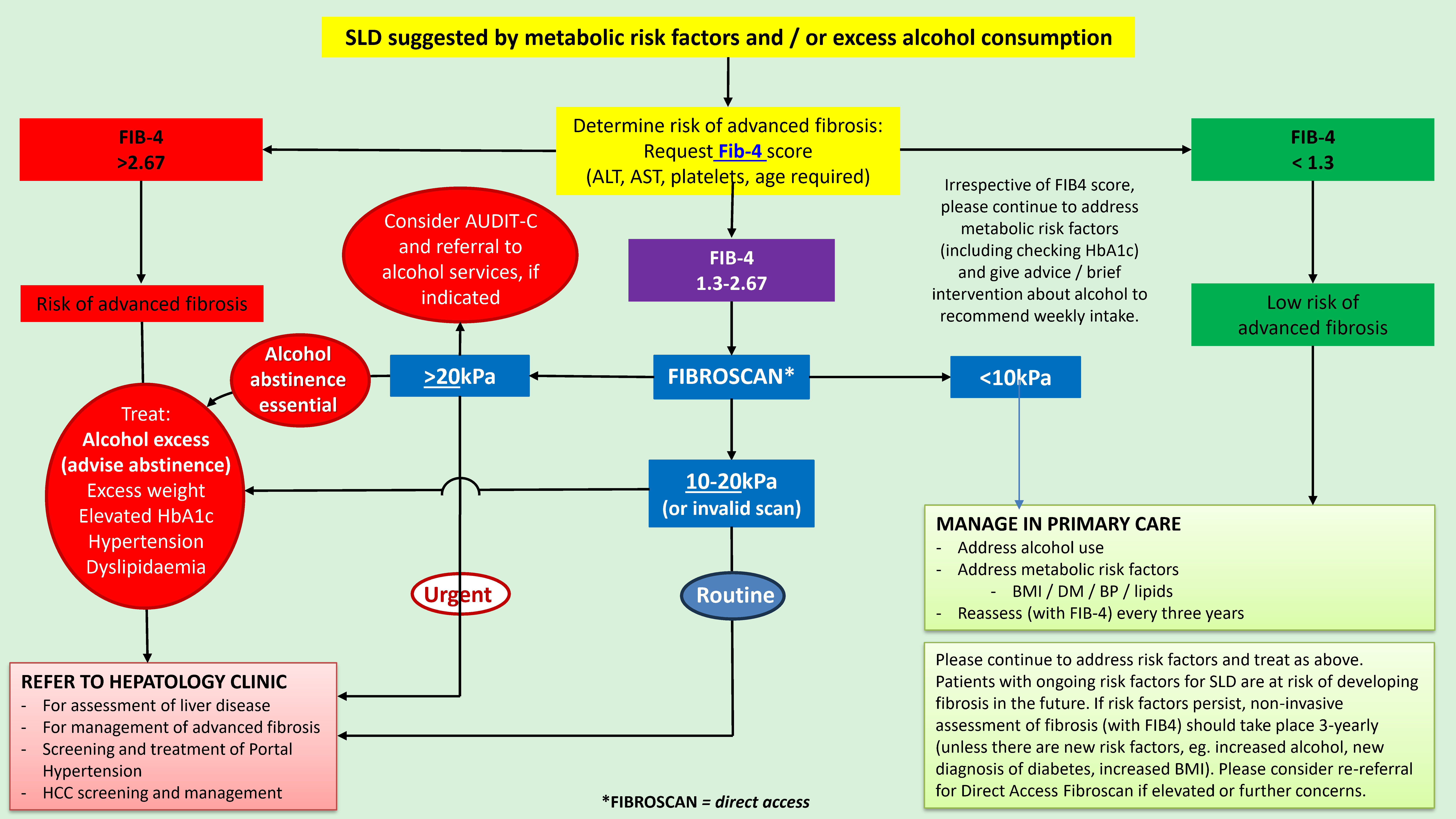
Steatotic Liver Disease (SLD)
Consider MASLD, Metabolic dysfunction and Associated Steatotic Liver Disease if patients have one or more of:
- Overweight or obese
- Diabetes
- Hypertension
- Dyslipidaemia
Consider alcohol related disease if people drink more than 14 units/week.
Consider screening for cirrhosis in people who drink above:
- Men: 50 units/week
- Women: 35 units/week
Steatotic Liver Disease (formerly known as ‘Fatty Liver Disease’) is the main cause of chronic liver disease (advanced fibrosis / cirrhosis) in the UK.
SLD is caused by excess alcohol consumption (>14 units / week) and / or metabolic risk factors (BMI >25, diabetes, hypertension, dyslipidaemia).
- Addressing these risk factors is central to prevention of chronic liver disease.
- Ultrasound may be unreliable at detecting (or excluding) steatosis, fibrosis, or cirrhosis, unless there are overt features of advanced cirrhosis (e.g. splenomegaly or ascites)
- Investigation and monitoring should focus on the identification of advanced fibrosis / cirrhosis.
- Other causes of steatotic liver disease (e.g. drugs or cryptogenic steatotic liver disease (‘lean’ MASLD), in which there are no metabolic risk factors) should prompt Hepatology A&G / referral.
New definitions:
- MASLD: Metabolic dysfunction associated steatotic liver disease [formerly NAFLD ‘non-alcoholic fatty liver disease’]
Metabolic risk factors and low alcohol intake
- MetALD: Metabolic and alcohol-related liver disease
Metabolic risk factors and moderate alcohol intake (15-45 units/ week)
- ALD: Alcohol-related liver disease
Alcohol >45 units/ week
Steatotic liver disease (SLD) is the most common cause of abnormal liver enzymes
- Screen for SLD: alcohol history, BMI, HbA1c, metabolic risk factors
- Assess Fibrosis risk in SLD: FIB-4 -> Fibroscan -> referral if indicated
- Manage risk factors in SLD: Alcohol advice/ abstinence, address metabolic risk factors
- Repeat Fibrosis risk assessment in 3 years (FIB-4)
- Advise 10% weight loss if obese
- Treat diabetes if HbA1c elevated
- Address hypertension
- Address dyslipidaemia
- Advise abstinence from alcohol, regardless of aetiology
Use AUDIT-C to screen for harmful alcohol use.
- If appropriate consider alcohol services referral, including consideration of community-based medically assisted alcohol withdrawal where available (eg. via Change Grow Live
Non-Hepatic Causes
Thyroid disease
Elevated ALT and ALP are commonly seen at varying levels in active hyper- and hypo-thyroidism. Levels return to normal around 3 months after resolution of euthyroid state. In a well patient repeat at 3 months (and at 6 months if still abnormal).
Refer to Hepatology if:
- ALT remains elevated at 6 months.
Consider referring earlier patients with an ALT>150 and positive anti-smooth muscle or LKM antibodies or antimitochondrial antibodies, as these may be indicators of co-existent autoimmune liver disease.
Coeliac Disease
Coeliac disease (undiagnosed): Serum AST and ALT <150 IU/L with the ALT usually slightly greater than AST. Levels return to normal 3-6 months following a gluten-free diet.
In a well patient repeat at 3 and 6 months. P
atients with positive coeliac serology do not need referring to Hepatology
Refer to Hepatology if:
- ALT remains abnormal 3-6 months after commencing a gluten free diet
- Positive liver antibodies
Muscle Damage / Disease
High ALT may be seen in long distance runners, or patients with symptoms of myositis. Creatine kinase (CK) will also be elevated.
Symptoms of polymyalgia/myosis etc without risk factors for liver disease need urgent referral to Rheumatology.
Otherwise, treat the underlying problem and repeat the ALT at 3 months. Refer to Hepatology if ALT remains abnormal or not improving at that point.
Hepatitis
Viral Hepatitis
Hepatitis B – Request HBsAg (hepatitis B surface antigen).
Hepatitis C – Request HCV antibody. If positive, a fresh EDTA sample for PCR will be required.
Auto-Immune Hepatitis / Globulinaemia [2]
Auto-immune hepatitis [1]:
- Type 1 (formerly called lupoid):
- mainly found in young to middle-aged women
- Associated with high titres of anti-nuclear antibodies (ANA) and antismooth muscle antibodies (SMA), and raised IgG
- Type 2:
- mainly found in children
- associated with auto-antibodies against liver kidney microsomes (LKM1)
- Type 3:
- mainly found in young women
- associated with antibodies to soluble liver antigen and to liver and pancreas antigen
Autoantibodies can be negative in autoimmune hepatitis.
If IgG is elevated and clinical suspicion of autoimmune hepatitis, (eg. personal/ family history of autoimmune disease, female sex and absence of steatotic liver disease/ viral hepatitis), please consider A&G/ referral to Hepatology.
ANA is not specific for AIH and in the presence of a normal IgG and the absence of clinical suspicion of AIH, is unlikely to be clinically significant.
Genetic / Inherited liver disorders
Alpha-1 Antitrypsin Deficiency [2]
Incidence is around 1 in 3000 in the UK. Request alpha-1-anti-trypsin (AAT) levels. If low, send fresh serum sample for phenotyping, which is only indicated in patients with levels below normal or those with an affected first-degree family member.
Patients with alpha-1 antitrypsin deficiency (the PiZZ phenotype) may develop liver disease, but the spectrum stretches from liver failure requiring transplantation in childhood to chronic liver disease in adults.
High Alpha -1-antitrypsin (A1AT) are of no clinical concern.
Haemochromatosis
Ferritin can be difficult to interpret because it is an acute phase protein and is therefore a nonspecific screening test for haemochromatosis.
If elevated, refer to separate guidance.
Wilson's Disease [2]
Wilson's disease is an autosomal recessive disease, characterised by low caeruloplasmin. Do not screen for Wilson’s Disease in patients over 40 years of age.
Screening test is serum ceruloplasmin (not serum copper). Testing is only needed once in primary care. Please refer all patients with a low ceruloplasmin to Hepatology for further evaluation.
High caeruloplasmin levels are of no clinical concern.
Raised ALP
ALP comes from a variety of sources, but predominantly bone and liver. Increased levels may indicate:
Liver
- Bile duct obstruction
- Primary Biliary Cirrhosis
- Primary Sclerosing
- Cholangitis
- Drug-induced cholestasis
- Metastatic liver disease
- Heart failure
Placental
- Pregnancy
Bone
- Bone growth (children & adolescents)
- Vitamin D deficiency
- Healing fractures
- Bone disease, e.g. Pagets
- Bone metastases
Intestinal
- Non-fasting healthy individuals with blood group O or B
DRUGS THAT CAUSE INCREASES IN ALP:
- Antibiotics: penicillin derivatives, nitrofurantoin, erythromycin, aminoglycosides, sulfonamides, trimethoprim-sulfamethoxazole
- Antiepileptic drugs: carbamazepine, phenobarbital, phenytoin, valproic acid
- Antihistamines: Cetirizine
- Cardiovascular drugs: captopril, diltiazem, felodipine, verapamil, quinidine, flutamide
- Disease modifying agents: penicillamine, sulfa drugs, gold salts
- Polycyclic aromatic hydrocarbons: oestrogens, anabolic steroids, steroids, methyltestosterone
- Psychotropic drugs: monoamine oxidase inhibitors, phenothiazines e.g. chlorpromazine
- Diabetes drugs: tolbutamide, chlorpropamide, tolazamide
- Other drugs: allopurinol, methimazole, disulfiram, phenylbutazone
(See also flowchart B & C below)
Isolated ↑Bilirubin
Raised bilirubin can be the result of impaired excretion or raised production:
- Raised production can be the result of obstructive liver disease
- Other liver enzymes (alkaline phosphatase and gamma-GT) are usually increased
- Typically more than 50% of the bilirubin is conjugated bilirubin
Isolated raised levels of unconjugated bilirubin is typically due to in vivo haemolysis, or a defect in conjugation of bilirubin e.g. in Gilbert's disease.
- If haemolysis is suspected, check reticulocyte count, blood film, haptoglobin and lactate dehydrogenase
Bilirubin <30umol/L
- Well patient – repeat in 3 months
- Suspicion of haemolysis – check haptoglobin, LDH, FBC and reticulocytes. (Conjugated (split) bilirubin will not be informative at this level)
Bilirubin 30 – 60umol/L
- Check reticulocyte count, haptoglobin, LDH, FBC and conjugated (split) bilirubin (not always informative at this level)
- Gilbert's syndrome is probable if >70%, unconjugated (and no evidence of haemolysis): no further testing needed if non-progressive on interval retesting
- If haemolysis is suspected then Haematology referral
- If conjugated bilirubin > 50% then Hepatology referral to exclude rare causes such as Dubin-Johnson syndrome and drug induced
Bilirubin >60umol/L
Probable liver obstruction. Isolated raised bilirubin at this level would be unusual.
- Check conjugated (split) bilirubin
Further investigation required:
- If haemolysis is suspected then Haematology referral
- If conjugated bilirubin > 50% then Hepatology referral
Referral Criteria/Information
|
Aetiology tests |
If abnormal? |
|
Ultrasound of liver and upper abdomen |
Refer to Actions following an abnormal liver ultrasound scan |
|
Hepatitis B surface antigen |
Refer to Hepatology |
|
Hepatitis C antibody |
Send fresh EDTA sample for PCR |
|
Liver autoantibodies (ANA, AMA, LKM, SMA) |
Refer to Hepatology |
|
Immunoglobulins (IgA, G, M) |
Refer to Hepatology unless the only abnormality is mild elevation of immunoglobulins (polyclonal or IgA alone) in someone with a clear alcohol history. |
|
Clotting (only if patient is jaundiced) |
Refer to Hepatology |
|
AST |
AST / ALT ratio >2 suggests alcoholic liver disease. Refer to SLD pathway |
|
Alpha-1-antitrypsin (AAT) |
High result – of no significance |
|
Caeruloplasmin (only if <40 years) |
High result – of no significance |
|
Ferritin |
High result – check fasting iron saturation and follow guidance |
|
Thyroid Function Tests (TFTs) |
Manage in Primary Care and follow guidance |
|
Coeliac serology (tTG) |
Manage in Primary Care and follow local guideline |
|
HbA1c |
Manage in Primary Care |
|
Full Blood Count |
Manage according to results |
Actions following an abnormal liver ultrasound scan (USS)
|
Overt features of cirrhosis (e.g. splenomegaly, ascites, varices, nodular liver) |
Refer to Hepatology AND Address risk factors |
|
Features of steatotic liver disease |
Perform non-invasive tests of fibrosis AND Address risk factors |
|
Gallstone disease / gallbladder polyps |
Refer to General Surgery |
|
Possible malignancy |
Refer via Upper GI 2WW pathway |
Risk factors:
- Advise abstinence from alcohol (refer to alcohol services, if appropriate)
- Weight management
- Optimise glycaemic control (if diabetic)
- Optimise anti-hypertensive control
- Optimise lipid profile
Medications
Take a full medication history, remembering to ask about:
- Over-the-counter medications
- Herbal preparations
- Chinese medicines
- Illicit drugs
- Anabolic steroids and other performance enhancing drugs, e.g. gym supplement
If there is a clear temporal relationship with other drugs (e.g. antibiotics) stop the drug and monitor for improvement. If ALT>150U/L or patient jaundiced, refer to hepatology (urgently if jaundice present). Otherwise, monitor to establish normalisation, with A&G to Hepatology if no improvement.
Almost any medication can cause an elevation of liver enzymes, particularly:
- NSAIDs
- Antibiotics
- Statins - A mild rise in ALT is common after starting a statin. If the pretreatment ALT was abnormal seek a cause. If it was normal and rise is under x3ULN, continue statin and monitor.
- Anti-epileptic drugs (AEDs)
- Anti-tuberculous medications (discuss with supervising respiratory consultant/infectious disease consultant)
Additional Resources & Reference
Primary care guides
Liver disease and liver blood tests - a guide for primary care *Completely updated guidance - September 2025*
Hepatitis C treatment services basic fact sheet
Patient Information Leaflets/ PDAs
The British Liver Trust website contains information on a wide range of liver disease and risk factors.
References
[1] Contributors representing the Royal College of Physicians (RCP); 2011.
[2] Dufour DR. Laboratory guidelines for screening, diagnosis, and monitoring of hepatic injury. Clin Chem 2000; 46: 2027-49.
Associated Policies
Places covered by
- North Yorkshire
- Vale of York
Hospital Trusts
-
York and Scarborough Teaching Hospitals