Haemochromatosis
Definition/Description
Genetic haemochromatosis (GH) is a recessive genetic disorder characterised by continuous absorption of iron from the gut. This can result in iron accumulation and systemic tissue damage, including liver cirrhosis and diabetes mellitus. Early detection can prevent organ damage and increase life expectancy. Defects of the HFE gene (located on the short arm of chromosome 6) cause the majority of cases of inherited haemochromatosis, which is therefore often referred to as HFE haemochromatosis (HFE-HC). HFE was the only known gene associated with haemochromatosis but it is now known that there are other genetic associations where the HFE-HC gene test will be negative
Red Flag Symptoms
There are none as such though failure to diagnose and treat leads to advanced disease - including diabetes, bronzing of the skin, hepatomegaly and arthropathy, especially of the second and third metacarpophalangeal joints, Impotence, amenorrhoea or hypogonadism, cirrhosis, hepatocellular carcinoma, diabetes mellitus, cardiac disease (arrhythmias or cardiomyopathy) and neurological or psychiatric symptoms - impaired memory, mood swings, irritability, depression. Initial symptoms are usually vague and nonspecific - eg, fatigue, weakness, arthropathy affecting various joints, non-specific abdominal problems, erectile dysfunction and heart problems. HHC may be diagnosed incidentally - eg, following abnormal serum ferritin or LFTs.
Guidelines on Management
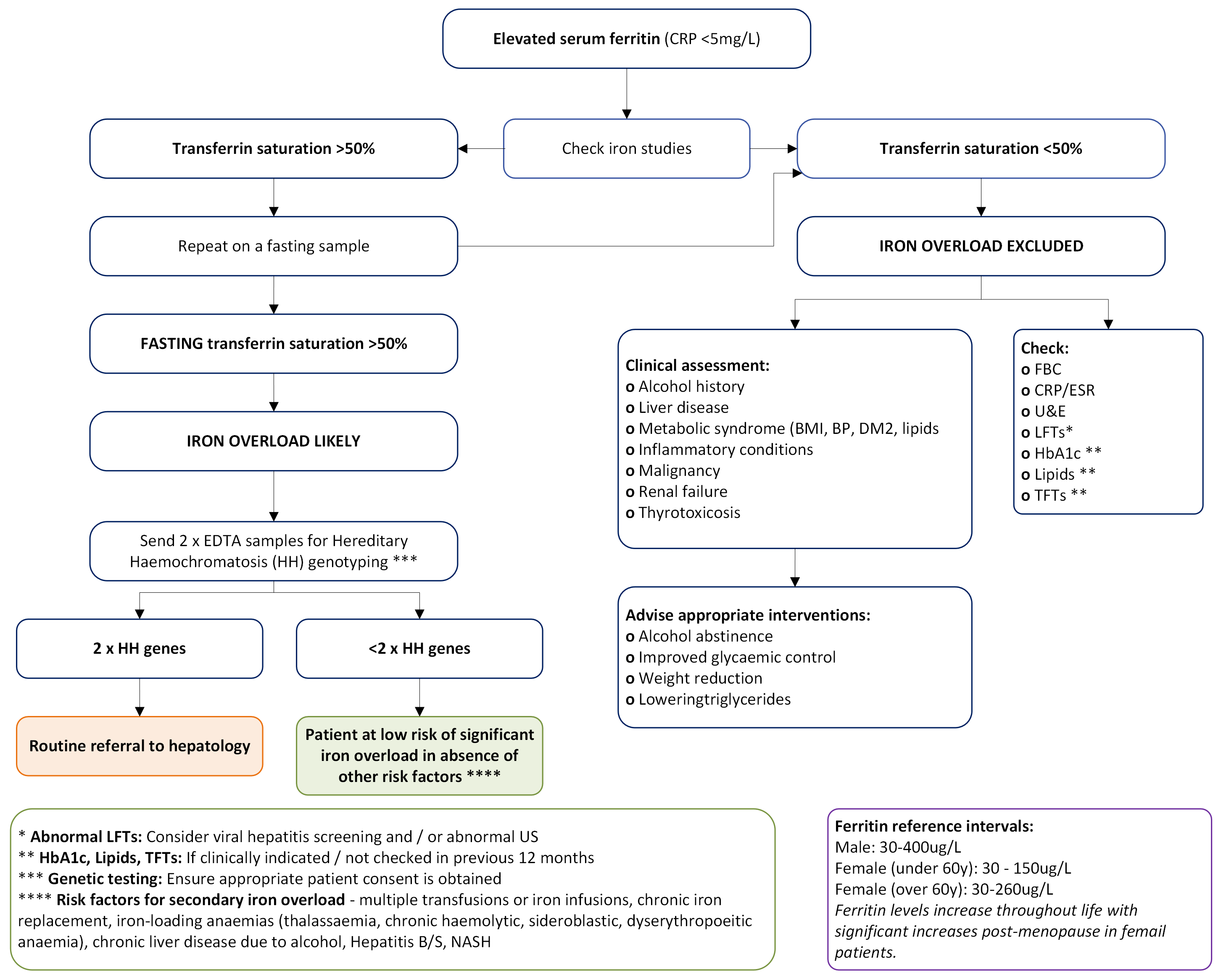
Unexplained high ferritin can be an incidental finding and may warrant further investigation. Only around 0.5% of these patients will have GH. Please refer to the following guidance for the investigation of raised ferritin below or link: https://tinyurl.com/BiochemInfo
Molecular testing for HFE related GH should be arranged only if the results are suggestive of iron overload:
- Elevated ferritin
- AND fasting transferrin saturation >50%
- WHEN the patient is not taking any iron supplements.
It is the responsibility of the requesting clinician to obtain appropriate informed consent prior to carrying out genetic testing as a genetic diagnosis may have implications for family members. Please refer to: https://patient.info/doctor/genetic-counselling-a-guide-for-gps
Outcome
If the fasting transferrin saturation or ferritin is not raised, iron overload is unlikely and genetic testing is not indicated. The laboratory will reject requests for genetic testing if the transferrin saturation is <50%, even in the presence of elevated ferritin.
In the context of elevated ferritin and transferrin saturation, patients found to carry two copies of the C282Y mutation (homozygotes), or one copy of the C282Y mutation and one copy of the H63D mutation (compound heterozygotes) should be referred to hepatology.
If this genetic susceptibility to GH is identified during family screening, but the ferritin/transferrin saturation is not raised, referral to hepatology is not required. Monitor serum ferritin every 1-3 years. Other heterozygous patients, i.e. carriers of one copy of the C282Y mutation, are not at risk of iron overload secondary to haemochromatosis and also do not require referral.
Referral Criteria/Information
Investigations prior to referral
- FBC, LFT, serum ferritin and fasting transferrin saturation
- HFE genotyping – patient consent required. This appears on ICE as Haemochromatosis Gene Studies
Referral Criteria
- Only patients with genetically confirmed susceptibility to haemochromatosis (homozygous C282Y or compound heterozygous C282Y/H63D genotype).
- AND evidence of iron overload (elevated serum ferritin and transferrin saturation >50%).
Information to include in referral letter
- Biochemistry and genetic testing results
- BMI
- Alcohol intake
Additional Resources & Reference
Patient information leaflets/ PDAs
https://haemochromatosis.org.uk/
https://www.facebook.com/groups/haemochromatosis
https://www.youtube.com/watch?v=r7qUdDS21ak
https://www.britishlivertrust.org.uk/liver-information/liver-conditions/haemochromatosis/
References
Fitzsimons, E.J., O Cullis, J., Thomas, D.W., Tsochatzis, E. and Griffiths, W.J. (2018) Diagnosis and therapy of genetic haemochromatosis (review and 2017 update). British Journal of Haematology 181, pp. 293-303.
Malton, K. and Turnock, D. (2019) Reflective testing in the diagnosis of hereditary haemochromatosis: Results of a short retrospective study. Annals of Clinical Biochemistry [online]. DOI: 10.1177/0004563219827614
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals