Nocturnal enuresis
Definition/Description
Nocturnal enuresis (bedwetting) is involuntary wetting during sleep. It is considered normal up to 5 years and uncommon up to 10 years.
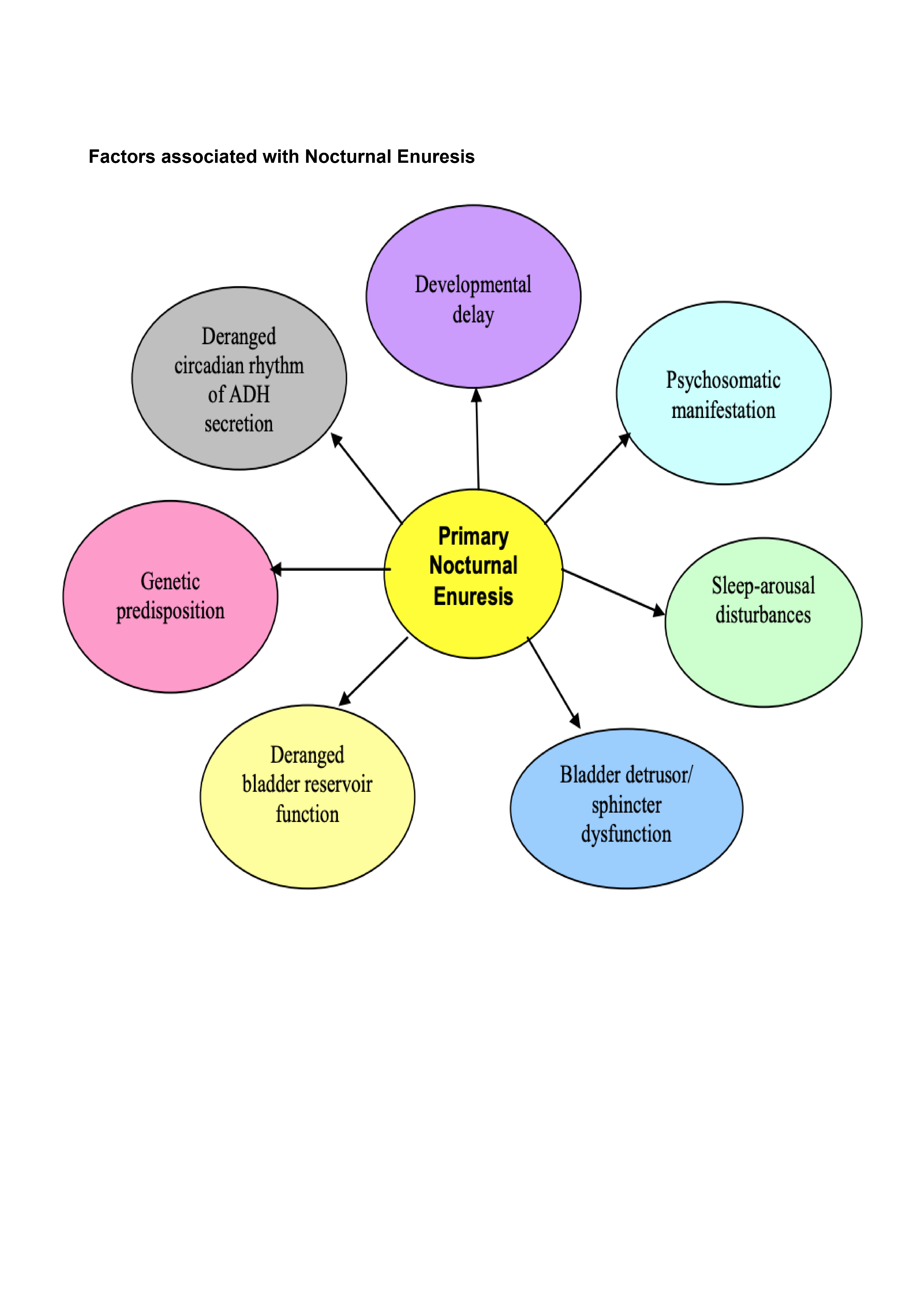
Primary nocturnal enuresis: recurrent involuntary passage of urine during sleep in children aged 5 or over, who has never achieved consistent night-time dryness. Often represents developmental delay which resolves over time.
This is divided into those with or without daytime symptoms such as urgency, frequency or daytime wetting.
Secondary nocturnal enuresis: involuntary passage of urine during sleep by a child who has previously been dry for at least 6 months. Requires the exclusion of underlying pathology.
Response to intervention: 14 consecutive dry nights or a 90% improvement in number of wet nights per week
Partial response: improved but 14 consecutive dry nights or 90% improvement in number of wet nights per week has not been achieved
Paediatric Normal Values (adapted from APLS) |
|||
Age |
Resp Rate |
Heart Rate |
Systolic BP |
Neonate <4w |
40-6 |
120-160 |
>60 |
Infant <1 y |
30-40 |
110-160 |
70-90 |
Toddler 1-2 yrs |
25-35 |
100-150 |
75-95 |
2-5 yrs |
25-30 |
95-140 |
85-100 |
Red Flag Symptoms
- Day and night symptoms: frequency, urgency, wetting
- Poor stream
- Dysuria
- Recurrent UTIs
- Safeguarding concerns
- Polydipsia, polyuria – consider diabetes
- Abdominal mass
- Abnormal spine/neurology – exclude occult spinal dysraphism or tethered cord (asymmetric/deviation of gluteal cleft)
Guidelines on Management
General Points
- Widespread and distressing condition that can have deep impact on the emotional, behavioural and social wellbeing of children
- Can be stressful for parents and carers
- Can limit the child’s social life and experiences, e.g. sleepovers, school trips
- May generate negative emotions and behaviours for the child, this may include helplessness, a lack of hope, an awareness of being different from peers, guilt and shame, humiliation, victimisation, and loss of self esteem
- Parents may feel frustrated and helpless
- More common in cases of neglect or abuse
- More common in boys (2:1)
- At age 5y, about 15% of children experience nocturnal enuresis
- There is a strong family predisposition (both parents = 77%, single parent = 43%)
- Only 1/3 affected will seek medical support
- It is very common, the prevalence decreases with age
Age (y) |
5 |
6 |
7 |
8 |
10 |
12-14 |
>15 |
Prevalence (%) |
16 |
13 |
10 |
7 |
5 |
2-3 |
1-2 |
History
- Onset of nocturnal enuresis – if very recent consider whether this is a part of a systemic illness
- Previously dry at night without assistance for 6 months
- Presence of day time symptoms such as frequency, urgency, polyuria, dysuria, poor urinary stream or straining – suggests overactive bladder or rarely an underlying urological disease
- Bedwetting pattern; nights per week, amount, time of night, arousal from sleep
- Large volume in first few hours of night is typical
- Variable volume of urine, often more than once per night, may also have daytime symptoms – consider overactive bladder
- Every night – severe, less likely to resolve than infrequent bedwetting
- Fluid intake; how much do they drink, are they drinking less because if bed wetting, caffeine containing drinks, polydipsia
- Bowel habit; constipation, soiling
- Sleeping arrangements; own room, snoring, disturbed sleep
- Do they have easy access to a toilet at night
- Consider proximity to parents for support
- Consider developmental or behavioural problems, diabetes mellitus or sleep apnoea
- Family history of renal problems or bed wetting
Examination
- Check growth
- Abdominal examination – distended bladder, faecal mass
- Check lumbosacral spine for swelling, tuft of hair suggesting spinal dysraphism
- Lower limb neurological examination including tone, power and reflexes
- Visual inspection of perineum
- DO NOT perform a digital rectal examination
Differential Diagnoses
- Urinary tract infection – daytime wetting with frequency and urgency
- Constipation and/or soiling
- Diabetes mellitus – polydipsia, weight loss, polyuria
- Developmental delay, attention or learning difficulties
Investigations
Usually investigations aren’t indicated for primary nocturnal enuresis, therefore most children will not require any investigations.
The following can be considered
- Urinalysis: new onset bedwetting, daytime symptoms, signs of illness, unresponsive to treatment
- Ultrasound with post-void volumes: daytime symptoms, unresponsive to treatment, poor stream, palpable bladder
Management
Refer to health child team for first line assessment and advice
Key principles
- Discuss with parents/carer whether they need support
- The management plan should be tailored to the individual child
- Reassure many children under 5 years wet the bed
- Advise parents/carers to take their child to the toilet if they wake during the night
- Suggest a trial of 2 nights in a row without nappies for a child who has been toilet trained during the day for 6 months
- Explain the important of appropriate fluid intake and using the toilet to pass urine regularly during the day and before sleep (4-7x/d); this helps to train the bladder to hold larger volumes
- Consider whether emotional or behavioural problems need the involvement of a professional with psychological expertise
- Treat constipation if present
- Both parent and child must be motivated before starting behavioural interventions
Fluid intake
- Amount of fluid needed varies according to the ambient temperature, dietary intake and physical activity
- Advise against fluid restriction
- Avoid caffeine-based drinks
Age (y) |
Gender |
Water from drinks (ml)* |
4-8 |
All |
1200 |
9-13 |
Girls |
1600 |
Boys |
1800 |
|
14-18 |
Girls |
1800 |
Boys |
2600 |
*Adequate intakes and not specific requirements
Behavioural
- Adapted to stage of development
- Include encouragement and reward systems
- Rewards should be given for agreed behaviour rather than dry nights,
- Drinking recommended fluid levels during the day
- Using the toilet to pass urine before sleep
- Engaging in management, such as taking medication or changing bedding
- Previously gained rewards should not be removed
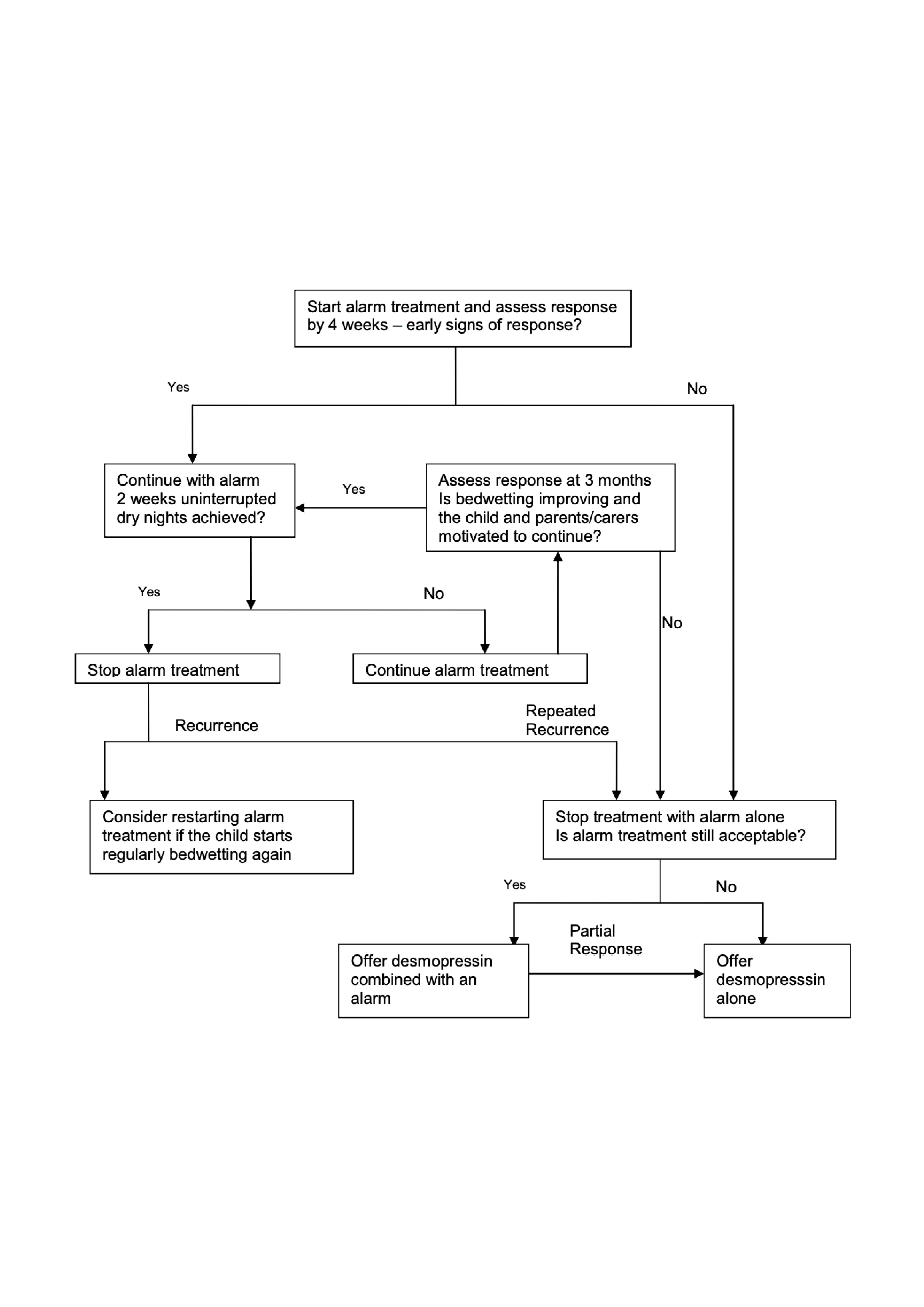
Alarm Treatment
- The most useful and successful way to treat bedwetting
- It may take 6-8 weeks to work
- Recommended from 6y onwards, depending on physical ability, maturity and motivation
- Children should be ‘in charge’ of their alarm and may need to be woken initially to turn the alarm off
- It is critical the child is fully awake during the process of going to the bathroom
- Reward systems can be useful during alarm therapy to reward behaviours such as
- Waking up when the alarm goes off
- Going to the toilet
- Returning to bed
- Resetting the alarm
- If the child is showing signs of response after 4 weeks, continue treatment until 2 weeks of uninterrupted dry nights are achieved
- Discontinue if not improvement within 4 weeks
- Alarm use can be restarted immediately without consulting a healthcare professional, if bedwetting starts again after stopping treatment
Desmopressin Treatment
Desmopressin is a synthetic analogue of vasopressin with an anti-diuretic action, which results in decreased urine production and increased urine concentration.
- It can be used in children >5y
- Relapse rates are high; 60-70%
Indications
- Alarm therapy has failed or is not suitable
- If rapid onset/short-term improvement is a priority of treatment
Sublingual desmopressin oral lyophilisates
>5y, initially 120 micrograms at bedtime; if needed, after 1-2 weeks increase to a maximum of 240 micrograms at bedtime
Or
Oral desmopressin tablets
>5y, initially 200 micrograms at bedtime, if needed, after 1-2 weeks increase to a maximum of 400 micrograms at bedtime
• Restrict fluid from 1h before dose until 8h after dose
• Assess response after 4 weeks (if no response, consider stopping)
• Withdraw for at least 1 week every 3 months to assess for relapse and ongoing need for medication
• Stop if fever or diarrhoea present
• Helpful for short term support, e.g. parental stress, trips away
Referral Criteria/Information
Indications for referral to bladder and bowel specialist nurses
- Primary nocturnal enuresis where red flags have been excluded
- AND little progress despite intervention and advice from the Healthy Child team
- Only available to Vale of York CCG patients
Indications for referral to paediatrics
- Unexplained persistent secondary enuresis
- Persistent enuresis with failure of an enuresis alarm
- Day-time enuresis or combined day/night enuresis after exclusion or treatment of a UTI and constipation
- History of recurrent UTIs
- Co-morbidity such as type 1 diabetes, physical or neurological problems
- Substantial psychological or behavioural problems
Information to include
- How long has problem been present?
- What treatment has been offered
- Any investigations and results
- Current medication
- Any developmental, attention or learning difficulties
- Any family problems
Additional Resources & Reference
Patient information leaflets/ PDAs
Patient info -childrens-health/bedwetting-nocturnal-enuresis
Nocturnal enuresis parent leaflet
References
- National Institute for Clinical Excellent [NICE] (2010) Bedwetting in under 19s: Clinical guidelines CG111 [Viewed 23 Aug 2021]
- National Institute for Clinical Excellent [NICE] (2020) Bedwetting (enuresis) [Viewed 23 Aug 2021]
- BNFc Nocturnal enuresis in children: Treatment summary [Viewed 23 Aug 2021]
- Kiddoo D; Nocturnal enureisis: non-pharmacological treatments. BMJ Clin Evid. 2015 Jan
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals