Management of suspected prostate cancer in primary care (before referral for secondary care assessment)
Definition/Description
Prostate cancer is a malignant tumour of the prostate.
- Almost all cancers of the prostate (95%) are adenocarcinomas (cancers of glandular cells).
- Multifocal — the different foci may be caused by different genetic mutations, which can differ greatly in growth rate and ability to metastasize. Most are indolent and grow slowly; a minority are aggressive in their tendency to invade local structures or to metastasize to remote tissues.
- Most common type of cancer in men — about 26% of all new cases of cancer in men are prostate cancer. Second most common cause of cancer death in males in the UK (after lung cancer), accounting for 13% of all cancer deaths.
- Curable - prognosis depends on the initial stage at diagnosis. The prognostic risk is calculated taking into account the prostate-specific antigen (PSA) level and staging, which is informed further using the Gleason score. The CORAL (Clinical Oncology Risk Assessment Library) Prostate app can help clinicians and patients with prognosis assessment.
Management
If the man has signs and symptoms which lead to a suspicion of prostate cancer:
Discuss the benefits and harms of PSA testing, and arrange for the test if appropriate. Offer a digital rectal examination.
Consider a DRE to assess for prostate cancer in men with
- Any of the symptoms above or
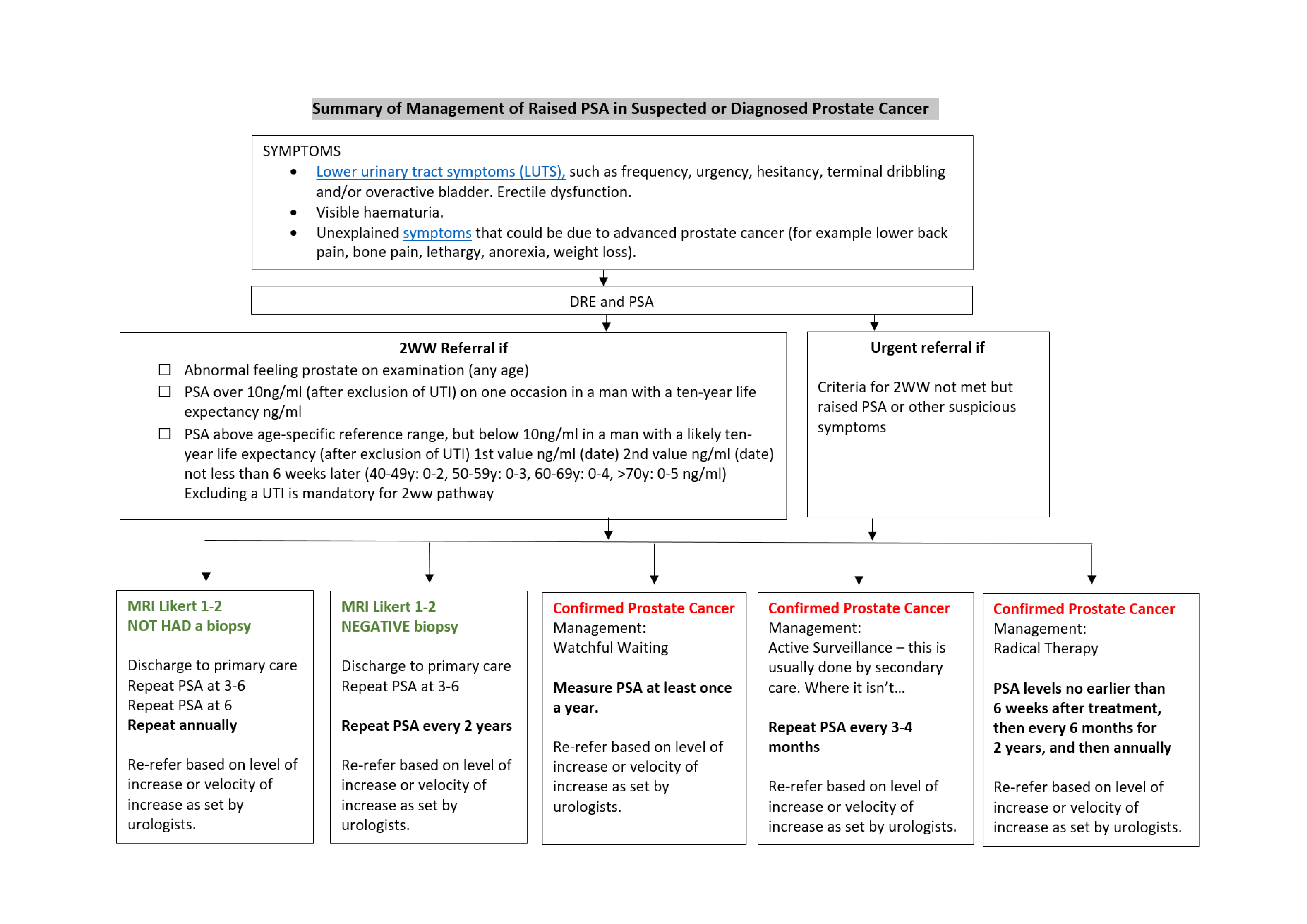
- Concerns about the possibility of prostate cancer, for example increased PSA levels. Follow up of patients diagnosed with Prostate Cancer – cross reference to other RSS The table on the next page summarises the management:
Red Flag Symptoms
Refer urgently using a suspected cancer pathway referral if:
- Digital rectal examination (DRE) reveals a hard, nodular prostate (suggestive of cancer) or
- PSA levels
- are over 10ng/ml (after exclusion of UTI) on one occasion in a man with a tenyear life expectancy or
- above the local age-specific reference range on two occasions six weeks apart: (40-49y: 0-2, 50-59y: 0-3, 60-69y: 0-4, >70y: 0-5 ng/ml) AND where a UTI has been excluded
Guidelines on Management
Risk factors
- Increasing age – mainly affects men aged over 50. Mostly a disease of older men (aged 65–79 years) but around 25% of cases occur in men younger than 65. (Autopsy studies - by the age of 80 years, 80% of men will have evidence of prostate cancer.)
- Black ethnicity - lifetime risk of being diagnosed with prostate cancer is 1:4 for black men, compared to 1:8 for white men. Black men also twice as likely to die of the disease.
- Family history of prostate cancer and genetics — increased risk depending on the number of relatives affected and the age at which they were diagnosed
- Weight — obesity and being overweight are associated with advanced prostate cancer. Lower testosterone levels increase the risk of more aggressive tumours; 15–20% increased risk of dying from prostate cancer with every 5 kg/m2 increase in BMI.
Diagnosis - suspect prostate cancer in men who have any of the following that are unexplained:
Symptoms:
- Lower urinary tract symptoms (LUTS), such as frequency, urgency, hesitancy, terminal dribbling and/or overactive bladder. These symptoms are common in older men and early prostate cancer does not usually cause LUTS. Localised prostate cancer is usually asymptomatic and localised advanced prostate cancer is also frequently asymptomatic. By the time prostate cancer causes LUTS, it may be advanced and incurable.
- Erectile dysfunction.
- Visible haematuria.
- Unexplained symptoms that could be due to advanced prostate cancer (for example lower back pain, bone pain, weight loss).
- Metastases may cause the first symptoms of prostate cancer, as they frequently metastasize to the bones, where they can cause pain, pathological fractures, or spinal cord compression.
Digital Rectal Examination (DRE) findings:
- A prostate that is hard and nodular on DRE — but a normal DRE does not exclude prostate cancer.
PSA levels:
- PSA levels that are raised, or rising (where urinary tract infection, recent ejaculation, prostate massage, cycling, or prostate biopsy as other possible causes have been excluded).
Referral Criteria/Information
Referral Information
Use the 2WW form for referrals Information to include in referral letter
- Symptoms, Family history, DRE findings
- PSA result and ideally FBC, U+Es, Bone Profile if not done recently
- Relevant past medical / surgical history
- Current regular medication
- BMI/ Smoking status
Additional Resources & Reference
Patient information leaflets/PDAs
- The NICE Guideline NG 131 has a lot of helpful information on the investigation and management of suspected and confirmed Prostate Cancer and prognosis depending on diagnosed severity that many patients will find helpful.
- NHS A-Z
- Cancer Research UK
- Prostate Cancer UK
- Macmillan Cancer Support
NICE Quality Standards for Prostate Cancer
Statement 1: People with prostate cancer have a discussion about treatment options and adverse effects with a named nurse specialist.
Statement 2: People with low-risk localised prostate cancer for whom radical treatment is suitable are offered a choice between active surveillance, radical prostatectomy or radical radiotherapy.
Statement 3: People with intermediate- or high-risk localised prostate cancer who are offered non-surgical radical treatment are offered radical radiotherapy and androgen deprivation therapy in combination.
Statement 4: People with adverse effects of prostate cancer treatment are referred to specialist services.
Statement 5: People with hormone-relapsed metastatic prostate cancer have their treatment options discussed by the urological cancer multidisciplinary team.
References
NICE NG131 Prostate cancer: diagnosis and management May 2019
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals