Hormone replacement therapy (HRT)
Definition/Description
Treatment used to help menopause symptoms.
Red Flag Symptoms
None provided
Guidelines on Management
Diagnosis
- The following can be diagnosed without laboratory tests in otherwise healthy women aged over 45 years with appropriate menopausal symptoms:
- Peri-menopause — if the woman has vasomotor symptoms.
- Menopause in women who have:
- not had a period for at least 12 months and are not using hormonal contraception OR
- symptoms without a uterus
The mean age for the menopause is 52.
- Follicular Stimulating Hormone (FSH) test to diagnose menopause should only be done in women:
- Aged <40 years where menopause is suspected
- Aged 40-45 years with menopausal symptoms, including a change in their menstrual cycle
- Aged >45 years exhibiting atypical symptoms (include anything other than classic menopausal symptoms)
Level greater than 30 mIU/mL indicates post menopause, should be taken on day 2-5 of cycle
In women taking hormonal contraception causing amenorrhoea (IUS, POP, nexplanon) take two levels 6 weeks apart to determine whether menopausal, in which case contraception can be stopped after 1 year if over 50y.
Some women may have normal levels of FSH during the menopausal transition, so this should not exclude peri-menopause as a cause of their symptoms.
- A pelvic examination should be performed only if clinically indicated and to exclude other possible causes of symptoms.
- Consider HRT to manage menopause symptoms including vasomotor symptoms, psychological symptoms (including low mood that arises as result of menopause) and altered sexual function. Urogenital atrophy alone only requires topical estradiol and can be used before the menopause but can also be used in some women in addition to systemic HRT.
- The benefits of HRT are likely to outweigh the risks for women with disruptive symptoms below the age of 60 years or with-in 10 years of menopause. o In women with premature ovarian insufficiency (premature menopause), systemic HRT is recommended, if not contraindicated, until at least the average age of natural menopause (51-52 years) to prevent the early onset of osteoporosis.
- HRT may be appropriate for prevention of osteoporosis related fractures in women below the age of 60 years or within 10 years of menopause in symptomatic women or if other bone protection medication is contraindicated.
Initiating and managing HRT
- Managing symptoms: Address modifiable lifestyle factors to reduce menopausal symptoms:
- healthy balanced diet, to maintain an appropriate weight
- consume adequate calcium intake (700mg/day)
- undertaking regular weight bearing exercise
- Advise and support women in smoking cessation and reducing alcohol intake
- Ensure other long-term conditions are managed appropriately and any treatment is optimised
- Avoiding triggers for hot flushes if experiencing them (spicy foods, alcohol etc.)
- Good sleep hygiene
- The option of taking HRT is an individual decision made after a consultation with the woman that addresses quality of life, health priorities, risks (including age and time since menopause), benefits and her personal preference.
- Consider HRT, if not contraindicated, for treatment of vasomotor symptoms, low mood arising as a result of the menopause (other causes should be ruled out), uro-genital atrophy (either topical alone or alongside systemic).
- Discuss effectiveness of HRT, risks, benefits, bleeding patterns, side effects.
- Check have up to date Blood pressure, BMI and family history of risk factors (osteoporosis, breast cancer and coronary heart disease)
- Do not routinely offer selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs) or clonidine as first-line treatment for vasomotor symptoms alone.
- Choice of route
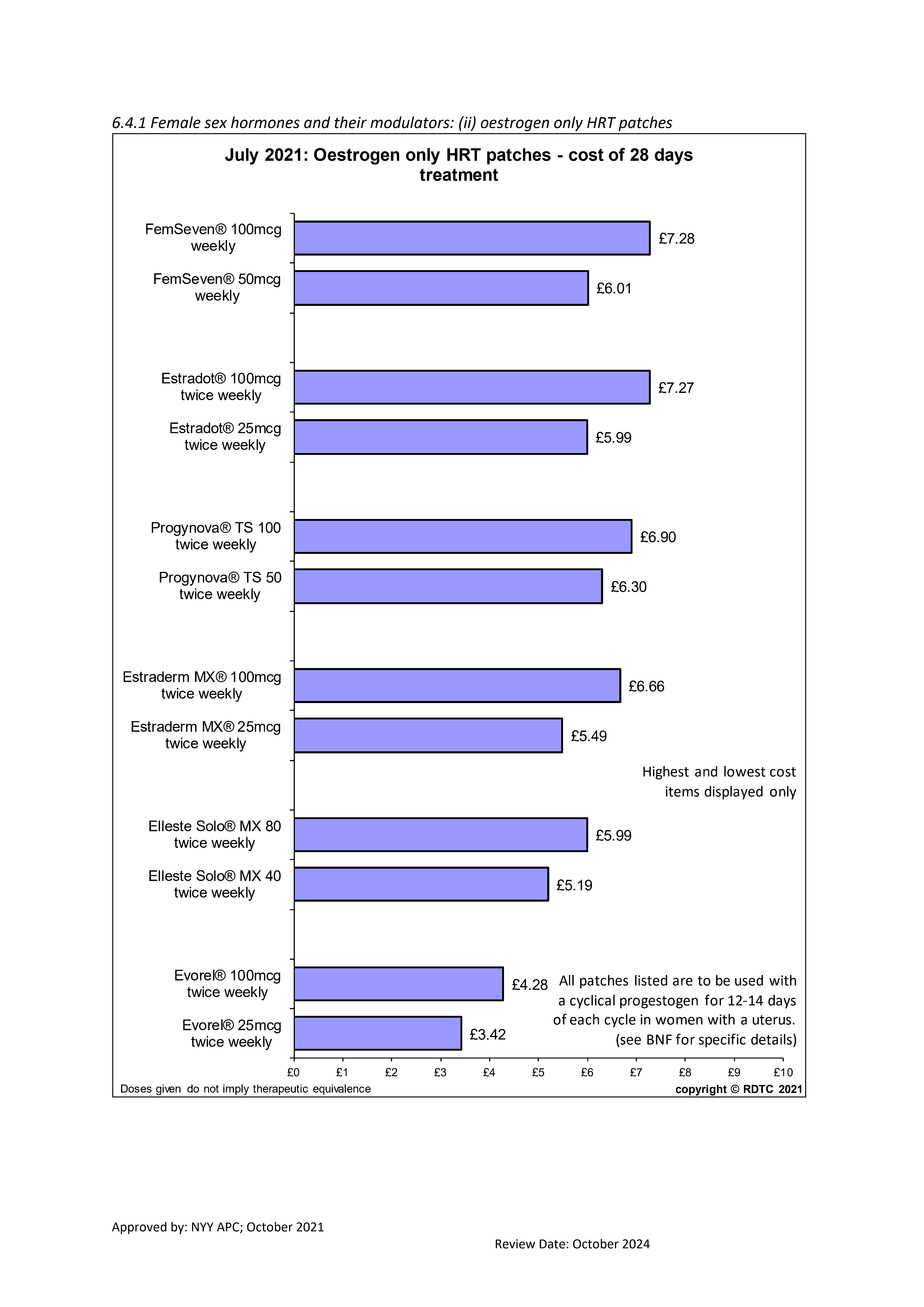
Offer patient choice of oral or transdermal. Note that there is lower risk of DVT with transdermal HRT compared to oral route, this may be the case as well for stroke especially when comparing to a low does patch preparation.
Avoid oral if:- VTE risks or personal history of VTE (both provoked and unprovoked consider referring to haematologist for advice before initiating any type of HRT.
- Poor symptom control with oral
- Bowel disorder /absorption problems /gastric banding,
- Lactose intolerance
- History of migraines
- Stroke risks e.g., BMI>30/smoker/sedentary
- History of or concerns of gall stones
- On hepatic enzyme inducing agent including OTC preparations
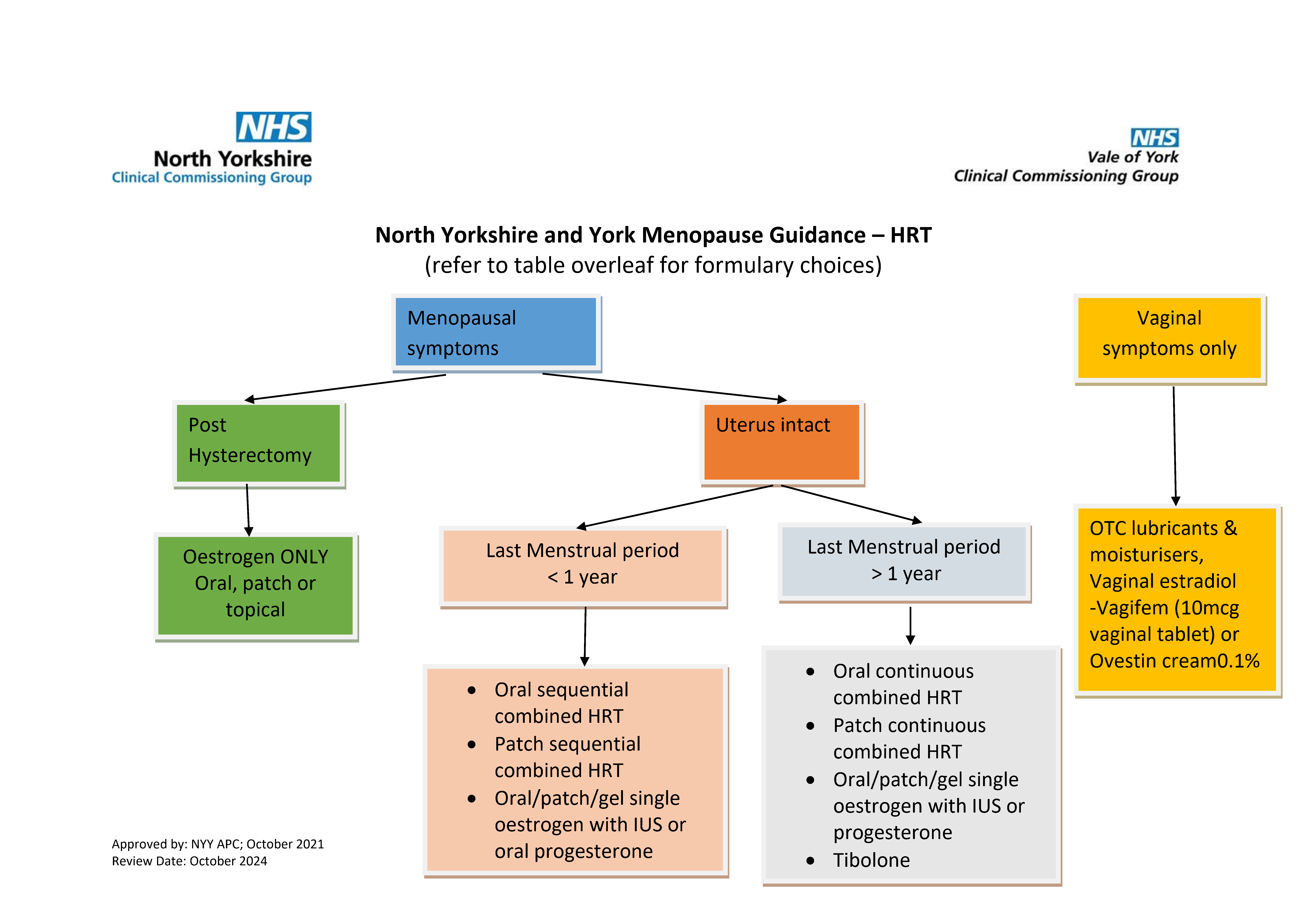
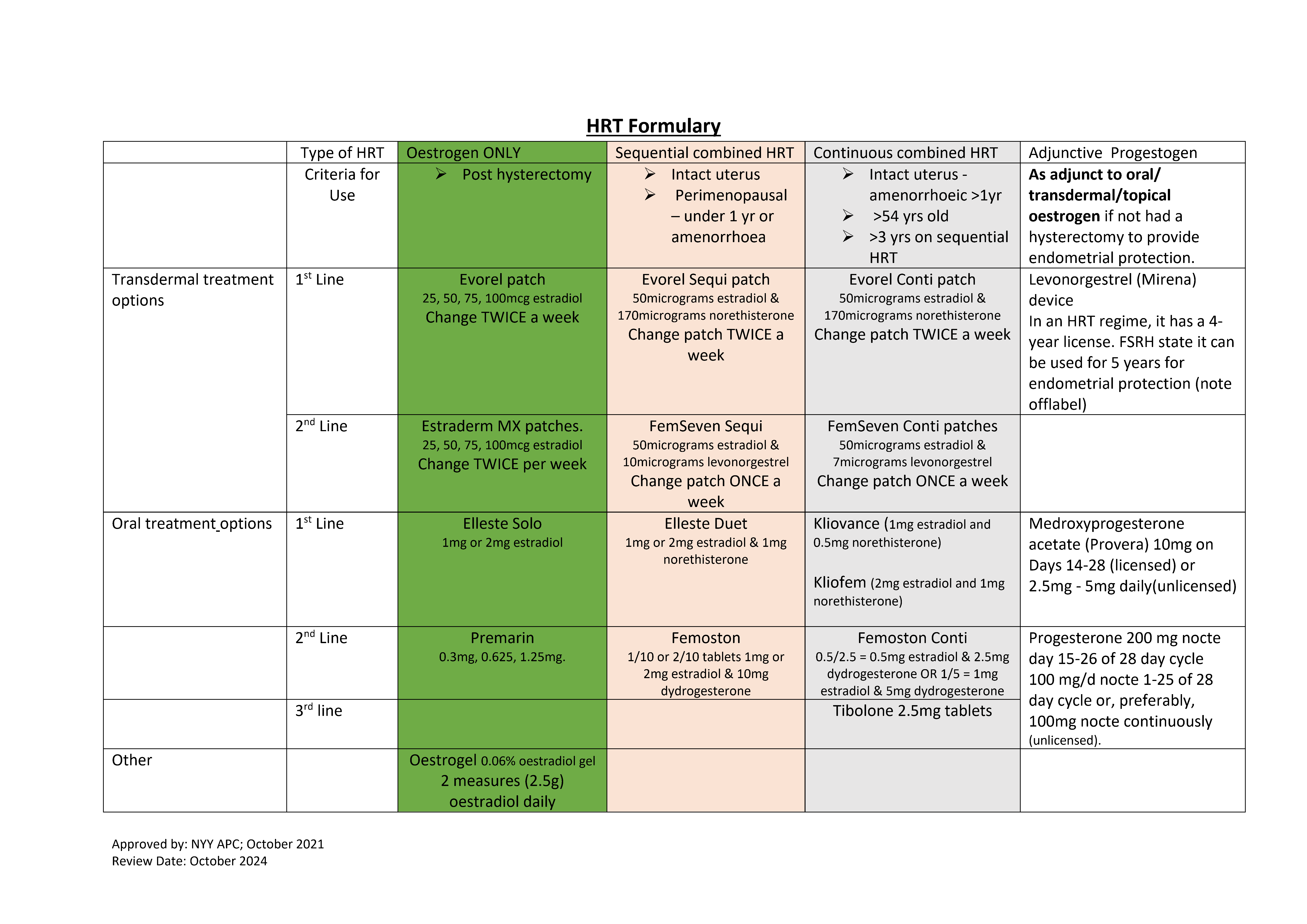
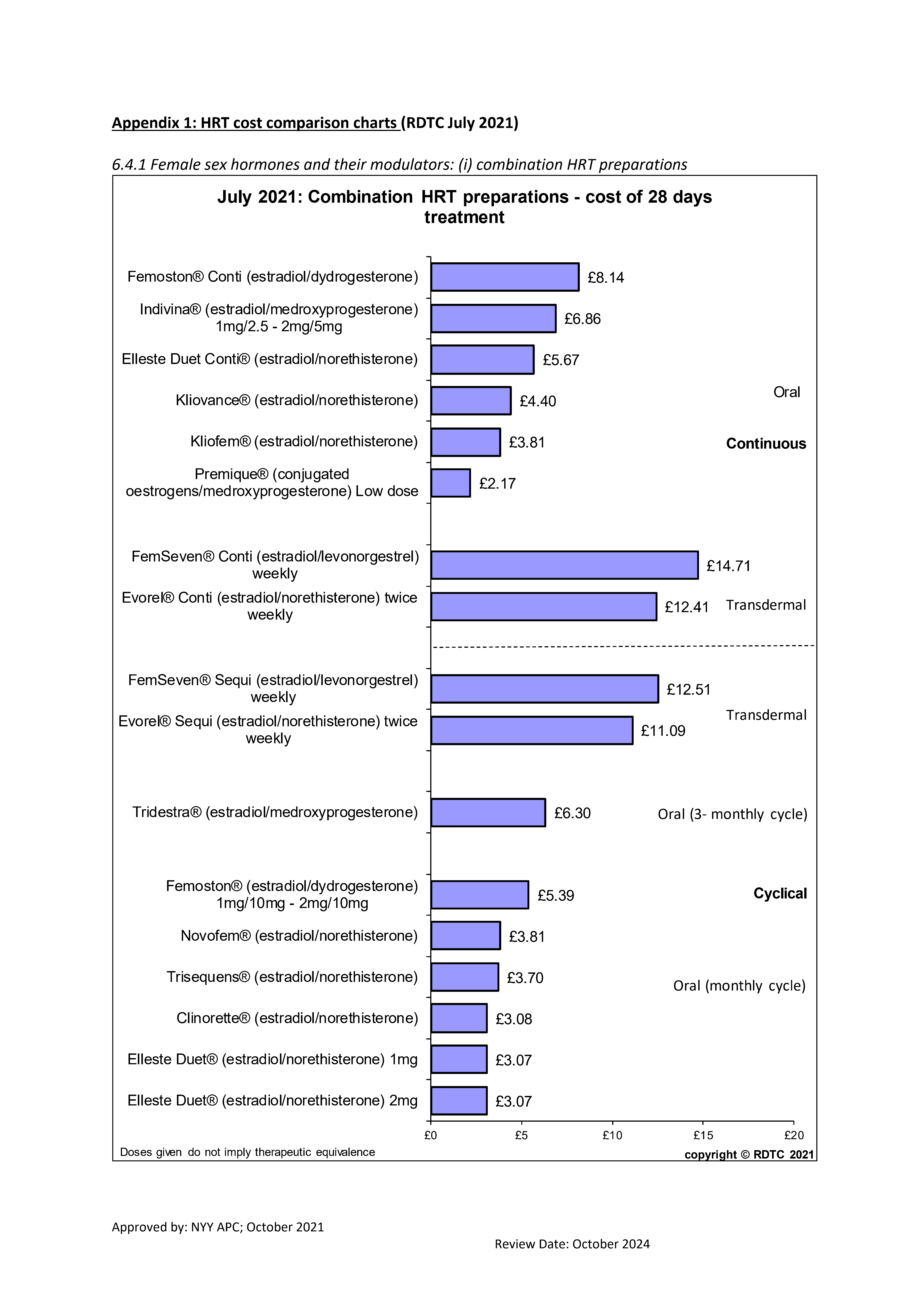
- Treatment regimens
Non-hysterectomised
Hysterectomised
Urogenital atrophy only
Perimenopausal
Postmenopausal
Oestrogen only
Low dose topical vaginal Combined cyclical (sequential) oestradiol or oestriol
Combined cyclical (sequential) regime (Note includes Oral/patch/gel single oestrogen with IUS or oral progesterone)
Cycle free HRT, continuous oestrogen and progestogen /progesterone
Continuous oestrogen/ cyclical progestogen for 10-14 days in 28 day cycle, giving cyclical progestogen withdrawal bleed. Consider changing to continuous combined HRT when postmenopausal or 54 years.
(Note includes Oral/patch/gel single oestrogen with IUS or oral progesterone)
Prescribe continuous combined (both oestrogen & progestogen)
- If history of severe endometriosis
- Subtotal hysterectomy
- TCRE (transcervical resection of endometrium)
Start early before irreversible changes have occurred. Can be taken whilst on systemic HRT (note latter is not required to specifically treat urogenital atrophy
- The dose and duration should be consistent with safety issues and treatment goals. Generally the lowest effective dose is advised for symptom control.
- Review after 3 months as symptom control and side effects (including bleeding) can take time to be effective and/or settle, then annually or earlier if concerns.
- Encourage women to maintain healthy diet and lifestyle, invite them to seek information at www.menopausematters.co.uk and www.nos.org.uk.
- Tibolone: It is a synthetic steroid with oestrogenic, progestogenic and androgenic activity so is a type of continuous combined HRT and so this is a no bleed preparation. Because of its androgenic activity, it has been shown to have a positive effect on libido. There is an increased risk of breast cancer and venous thromboembolism, broadly similar to combined HRT. Its use in women over 65 years needs to be cautious because of increased stroke risk.
- Follow-up/Annual Review/Duration of treatment
- Follow up after 3/12 of treatment to assess effect, enquire about side effects & bleeding pattern.
- Unscheduled vaginal bleeding is a common side-effect of HRT within the first 3 months of treatment but should be reported promptly if it occurs after the first 3 months (see recommendations on endometrial cancer in the NICE guideline on suspected cancer).
- Managing side effects: Encourage women to persist with treatment for 3 months (as adverse effects may resolve)
Side effects
Management strategies
Oestrogen related
Breast tenderness, GI side effects, Migraine, Leg cramps
Above side effects may occur continuously or randomly throughout the cycle
- Reduce dose
- Change route
- GI side effects: take with or after food
- Leg cramps may improve with lifestyle changes e.g. exercise, stretching calf muscles.
- Breast tenderness may be alleviated by a low-fat, high-carbohydrate diet.
- Migraine – switch to transdermal
Progestogen related
PMS type symptoms, Breast tenderness, Lower abdominal pain, Headache
Above side effects tend to occur in a cyclical pattern during the progestogen phase of cyclical hormone replacement therapy (HRT).
- Change type of progestogen
- Change route e.g. oral to transdermal
- Change regime - consider long cycle HRT or continuous combined HRT, perhaps with IUS to provide progestogen
- At annual review check efficacy, side-effects, ensure correct dose, optimal route of delivery and compliance. Also check:
- Pros & cons of continuing HRT, increased risk of breast cancer with long-term use, do benefits outweigh risks?
- Check blood pressure, encourage breast awareness/attendance of screening mammography
- Ensure cervical screening is up to date
- Assess osteoporosis risk & consider the need for investigation/monitoring Enquire about symptoms of urogenital atrophy
- Duration of treatment:
- Most guidelines recommend that HRT for around 5 years in women as they enter menopause (i.e. in late 40's/early 50's) is likely to confer benefit and not harm
- There are no reasons to place mandatory limitations on duration of HRT
- Guidance from the Committee on Safety of Medicine says:
- use the lowest effective dose of HRT to control menopausal symptoms
- use HRT for the shortest length of time
- Therefore it is important that the benefits and risks should be reassessed with each woman on an annual basis
- Withdrawing HRT slowly may reduce the chance of recurrent symptoms. It should be noted that 5% of women will have hot flushes for life
- Contraception and HRT: please see FSRH guidance (Contraception for Women Aged over 40 Years)
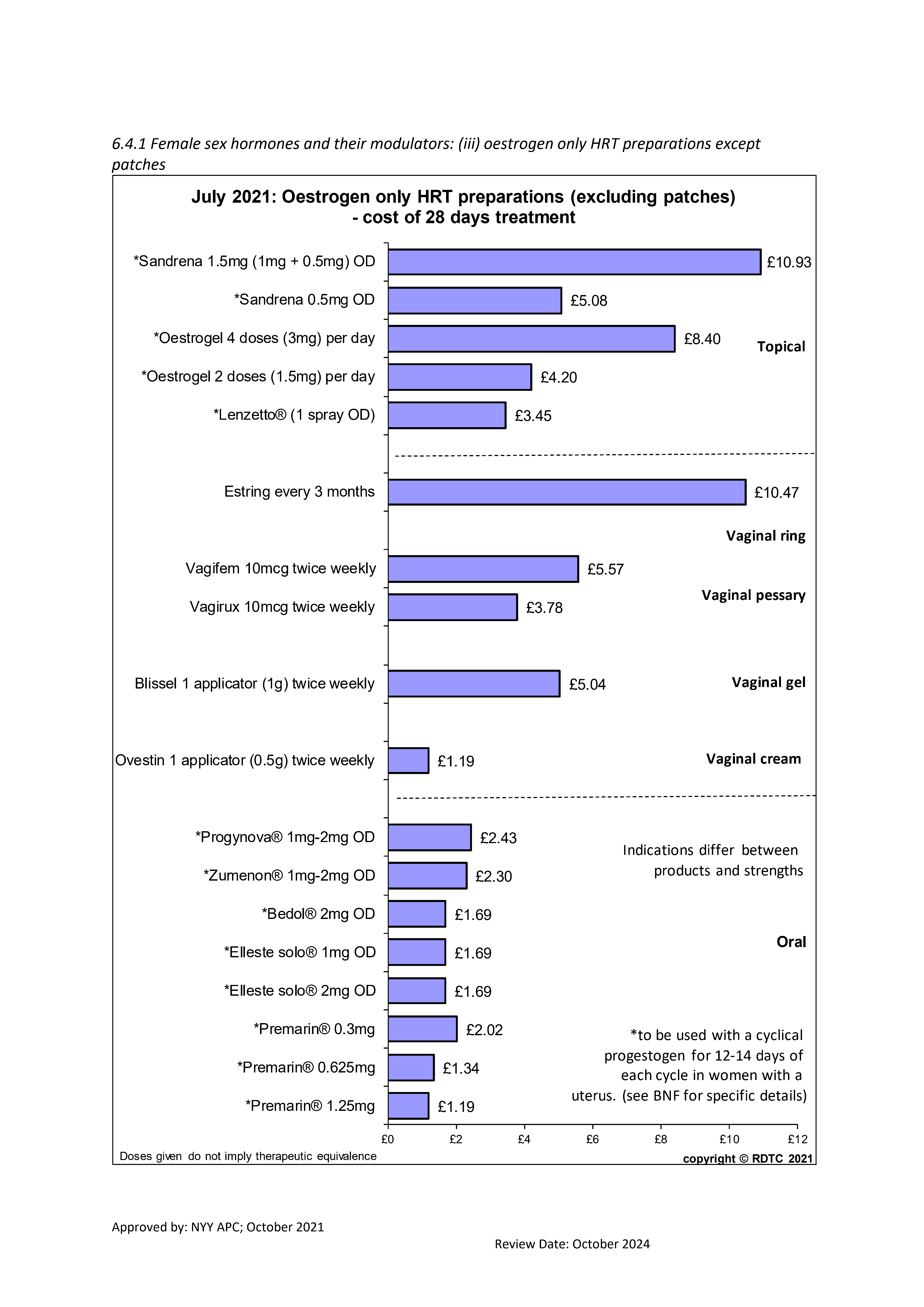
- Topical oestrogen for urogenital atrophy
- Offer vaginal oestrogen to women with urogenital atrophy (including those on systemic HRT) and continue treatment for as long as needed to relieve symptoms.
- Vagifem (10mcg vaginal tablet) or Ovestin cream0.1% are preferred options (NOTE Estriol 0.01% cream is 12 times more costly than estriol 0.1% (Ovestin®) cream but delivers an identical amount of estriol per application and therefore not on formulary).
- If vaginal oestrogen does not relieve symptoms of urogenital atrophy, consider other diagnosis such as Lichen Sclerosus or get further advice from a healthcare professional with expertise in menopause.
Contraindications and risks of HRT
Contraindications (see SPC for full details: http://www.medicines.org.uk/emc)
- Current, past, or suspected breast cancer.
- Known or suspected oestrogen-sensitive cancer.
- Undiagnosed abnormal vaginal bleeding.
- Untreated endometrial hyperplasia.
- Current venous thromboembolism (deep vein thrombosis or pulmonary embolism), unless the woman continues on anticoagulant treatment.
- Active or recent arterial thromboembolic disease (for example angina or myocardial infarction).
- Untreated hypertension.
- Active liver disease with abnormal liver function tests.
- Porphyria cutanea tarda.
- Pregnancy
- Dubin-Johnson and Rotor syndromes
Referral Criteria/Information
When to refer to specialist service
- Premature ovarian insufficiency/menopause. It is likely that most women <40 years will need referral to specialist clinic.
- Complex medical history
- concerns about the safety of HRT in a particular patient
- Persistent treatment problems e.g. side effects, lack of efficacy
- There is a sudden change in menstrual pattern, intermenstrual bleeding, postcoital bleeding, or postmenopausal bleeding — assess appropriately and arrange an urgent 2-week referral if a gynaecological cancer is suspected.
- History of hormone dependent cancer
Additional Resources & Reference
Patient resources
Rock My Menopause website (www.rockmymenopause.com) has a variety of factsheets and podcasts on various aspects of menopause.
Menopause Matters (www.menopausematters.co.uk) provides information on the menopause, menopausal symptoms, and treatment options.
Women's Health Concern (the patient arm of the British Menopause Society, website available at www.womens-health-concern.org) has a range of factsheets and an email advice service.
The Royal College of Obstetricians and Gynaecologists menopause Hub: www.rcog.org.uk/en/patients/menopause
The Daisy Network (www.daisynetwork.org) is a nationwide support group for women diagnosed with premature ovarian insufficiency or premature menopause.
https://patient.info/womens-health/menopause/hormone-replacement-therapy-hrt
References
NICE guidelines [NG23] Menopause: diagnosis and management, November 2015 (last updated 05 December 2019) https://www.nice.org.uk/guidance/ng23
NICE Clinical Knowledge Summaries Menopause last revised November 2020 http://cks.nice.org.uk/menopause The British Menopause Society: http://www.thebms.org.uk/ Menopause. NICE Quality standard [ QS143] Published date: February 2017 https://www.nice.org.uk/guidance/qs143
Menopause. NICE Pathway. Last updated: May 2021 https://pathways.nice.org.uk/pathways/menopause
FSRH Clinical Guideline: Contraception for Women Aged over 40 Years (August 2017, amended September 2019) https://www.fsrh.org/documents/fsrh-guidance-contraception-for-women-agedover-40-years-2017/
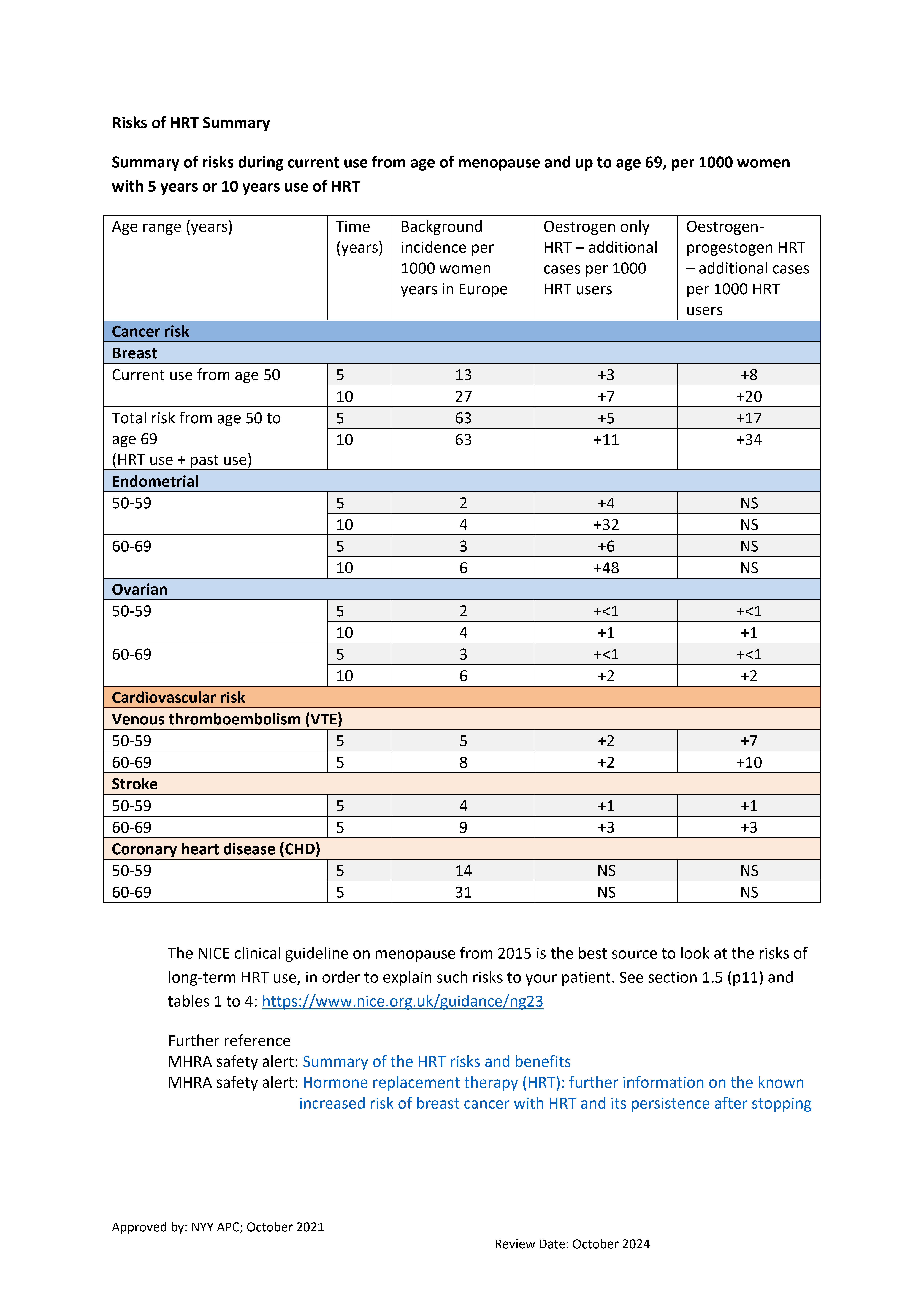
Further reference (see image C)
The NICE clinical guideline on menopause from 2015 is the best source to look at the risks of long-term HRT use, in order to explain such risks to your patient. See section 1.5 (p11) and tables 1 to 4: https://www.nice.org.uk/guidance/ng23
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals