Fibromyalgia
Definition/Description
Fibromyalgia is a pain syndrome comprising of widespread pain in muscles and joints, fatigue, non-restorative sleep and cognitive impairment, with an absence of findings on physical examination and in laboratory investigations that would explain symptoms.
Care should be taken to ensure other diagnoses are considered before making the diagnosis of fibromyalgia.
The predominant symptoms are those of pain and fatigue, commonly associated with disturbed sleep and low mood. There is an association with multiple other conditions e.g. depression, anxiety, IBS, Obstructive Sleep Apnoea, bladder irritability and restless legs to name a few.
Despite symptoms of soft tissue pain affecting the muscles, ligaments, and tendons there is no evidence of tissue inflammation.
Red Flag Symptoms
Usual indicators: Abnormal blood tests, Weight loss, Night pain
Guidelines on Management
Presenting features:
- More common in women, age 20 to 55
- Chronic, generalized pain: “hurts all over”, “like flu”
- Fatigue
- Non-restorative sleep
- Mood disturbances - 30 to 50% associated depression/ anxiety
- Cognitive disturbance - “fibro fog”
- Headaches - encountered in 50%
Examination:
- No inflammatory muscle or joint disease
Laboratory tests:
These are usually unremarkable and investigations should be kept to a minimum.
- FBC
- U+E
- LFT
- Bone profile
- CRP
- TFT
- Vitamin D
Diagnosis is based on clinical assessment and the above lab tests.
Classification criteria have been updated and old and new are outlined be
low for interest.
The 1990 ACR criteria for fibromyalgia advocated the use of tender points, with FM being diagnosed if >11/18 Smythe points are tender (see diagram), with widespread pain above and below the diaphragm, both left and right sides of the body. This is still widely used in practice.
The 2010 preliminary ACR criteria suggested use of the
- Widespread Pain Index (WPI) and
- Symptom Severity (SS) score, with
- symptoms at a similar level for more than three months, and
- absence of other diagnoses to explain symptoms.
This classification essentially does not require tender points on examination.
Widespread pain index (WPI) is based on sites of reported pain in the last three months, one point for each site, 19 maximum)
Neck |
Right Shoulder girdle |
Symptom severity score (SS)
Score these symptoms:
Symptoms |
Score |
|
Fatigue graded (0-3) |
0 = no symptoms |
|
Waking unrefreshed (0-3) |
||
Cognitive symptoms (0-3) |
||
Somatic symptoms in general – e.g. headache, low mood, anxiety, bladder symptoms, heartburn, IBS, etc |
|
|
Total |
A WPI score of 7 or above, or a SS score of 5 or above, or a WPI score of 3-6 with a SS score of 9 or above, would indicate fibromyalgia.
Management
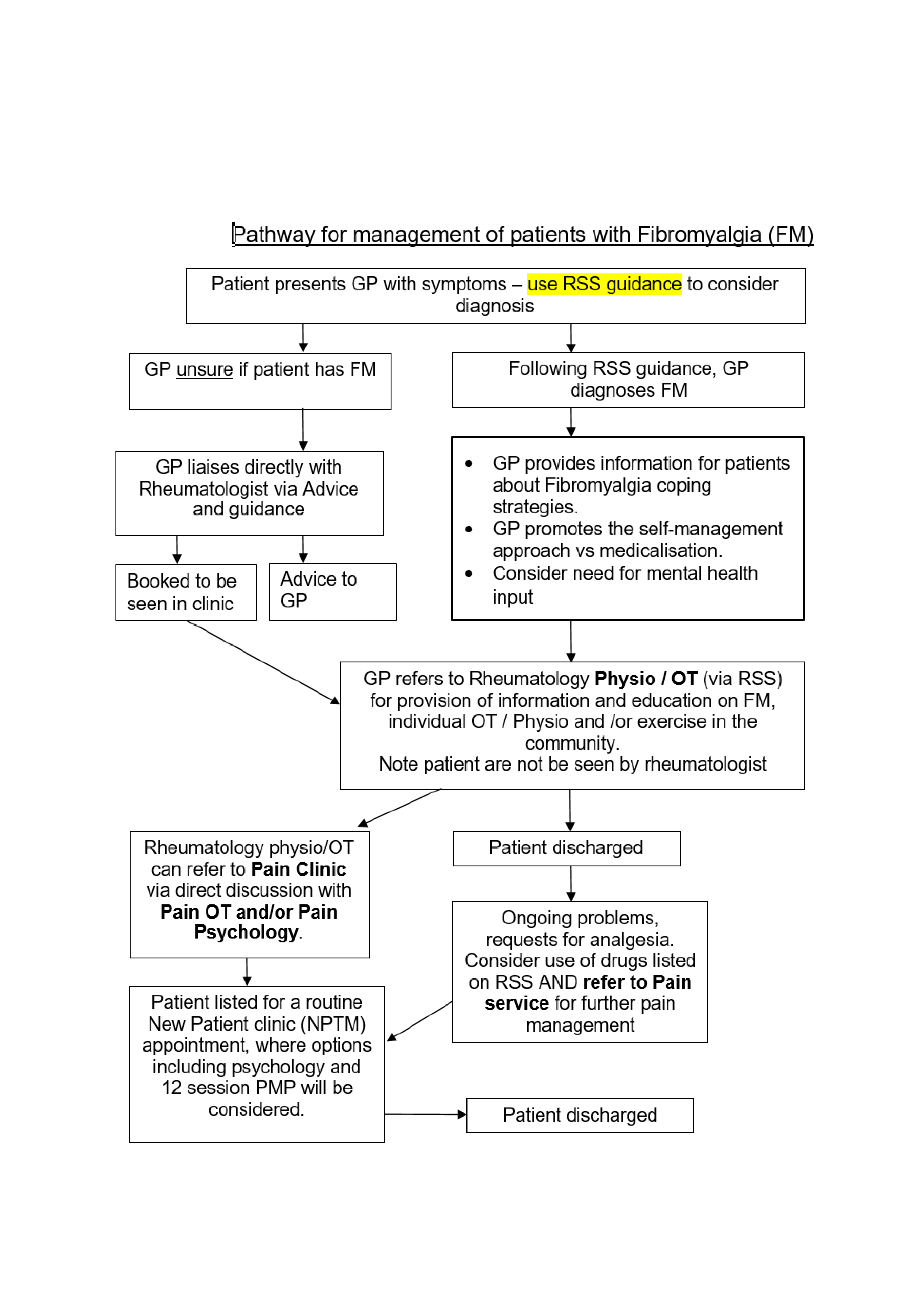
Fibromyalgia should be diagnosed and treated in primary care. Care should be taken to ensure other diagnoses are considered before making the diagnosis of fibromyalgia. GPs can do this as adeptly as specialists.
All patients should
- receive education regarding the condition.
- have their sleep addressed with advice regarding sleep hygiene, impact of sleep on pain etc.
- have an exercise program, including aerobic conditioning, stretching, and strengthening.
- have their mood assessed and referral to the mental health team considered if appropriate.
Patients with a diagnosis can be directly referred to York’s Rheumatology physiotherapy and occupational therapy service for support as the greatest evidence base for treatment and improving outcomes is for non-pharmacological interventions using a biopsychosocial model. The service aims to provide fibromyalgia patients with tools to self-manage their condition using pacing, relaxation, exercise, goal setting and sleep management.
Where patients have already had the 4 sessions of Rheumatology OT/physio support but are struggling to cope with their symptoms referrals can be made to the Pain Clinic (by GPs or the rheumatology team) who offer further psychological interventions for pain management and cognitive behavioural therapy.
Medication should only be used if the above have failed. It has a limited role in fibromyalgia and patients and prescribers should avoid using medication as a substitute for implementing the measures above or fulfilling a desire to be doing more.
Before starting any drug where the evidence for it use and benefit isn’t clear ask the patient ‘What’s the symptom(s) you would most like improved? Once they’ve listed each symptom ask them to score, for each, on a scale (0-10) how bad that symptom is now.
Agree with the patient whether 0 is no symptom or 0 represents their quality of life as a result of it. Decide a review period – one or two months would normally be sufficient, though there are some drugs the benefit of which takes longer. At the review time, without reminding the patient of how they scored last time, ask them about each symptom again and how they would score it now. This will help the patient reflect on how much, if any difference, does this drug really have. Where there’s no change, little change or the patient isn’t sure, (and let’s face it there are lots of reasons why on any one day we may feel differently), encourage patients to stop the drug and review how they are without it a few weeks later. There is little point in patients being prescribed drugs for which they are getting few clear benefits. Side effects and interactions may cause greater problems! Only by specifying symptom levels at the start, aligned with anticipated benefits will doctors and patients know whether there is any value in continuing them.
The following have been of benefit to some patients used usually as monotherapy.
- Amitriptyline
Not licensed for fibromyalgia. Licensed for neuropathic pain.
10mg £1.05 for 28
No monitoring required.
High doses associated with more side effects and care needed in the elderly because of anticholinergic side effects.
Start at 10mg daily taken between 6pm-8pm, titrate up as required to enable sleep and avoid daytime drowsiness. Usual dose range 20mg – 30mg daily.
- Nortriptyline
Not licensed for fibromyalgia, nor for neuropathic pain
10mg £1.32 for 28
No monitoring required
Less sedating than amitriptyline
Start at 10mg daily taken at night, titrate up to a maximum of 75mg daily as required to enable sleep and avoid daytime drowsiness.
- Duloxetine
Not licensed for fibromyalgia
30mg £1.65 for 28
Start at 30mg daily and increase to 60mg daily if needed
Referral Criteria/Information
Patients can be referred if there is diagnostic uncertainty.
Information to include in referral letter
- Length of history
- Distribution and severity of pain
- Extent of fatigue
- Sleep history
- Somatic symptoms e.g. “fibro fog”, IBS etc
- What other diagnoses you are querying or concerned about to warrant referral
- Comorbidities
- Confirmation all the listed blood tests are normal
Additional Resources & Reference
Patient information leaflets/ PDAs
Versus Arthritis Information on Fibromyalgia
NHS leaflet on Fibromyalgia
YHFT Physio and OT resource list
The following websites provide information regarding fibromyalgia, including advice around self management stratergies such as exercise, pacing, sleep and relaxation.
https://www.torbayandsouthdevon.nhs.uk/uploads/what-is-fibromyalgia.pdf
Information Around a Range of Self Management Stratergies
https://www.yorkhospitals.nhs.uk/your-visit/patient-information-leaflets/physiotherapy/
Follow the links to ‘Tips to Help With Memory Problems for Patients With Fibromyalgia’, ‘Relaxation and Wellbeing’, ‘Benefits of Exercise and Making it Part of Your Lifestyle, Pacing Activities and Goal Setting’,
http://my.livewellwithpain.co.uk/
Within the section ‘Resources for patients’, there are several different booklets you may find useful, including: ‘Goal setting’, ‘Pacing’, ‘Sleep Well with Pain’, ‘Ten Footsteps to Living Well with Pain’, ‘Your Journey with Pain’, ‘Sleeping Problems, An NHS Self Help Guide’
https://www.torbayandsouthdevon.nhs.uk/services/pain-service/reconnect2life/
This website contains useful resources including ‘Understanding Pain’, ‘Improving Health and Fitness’, ‘Changing the Way You Think & Feel’, ‘Reconnecting with Your Values’, ‘Creating Skills for the Future’
Information Regarding Excercise
Being physically active has enormous benefits for fibromyalgia, but many people find it difficult. This can be for any number of reasons, including pain, fatigue, fear, and lack of time or motivation. If you start a new exercise or activity you need to be guided by your own individual pain levels. Our advice would be to start gently and build up slowly using a graded approach. See Benefits of Exercise and Making it Part of Your Lifestyle, Pacing Activities and Goal Setting’ at https://www.yorkhospitals.nhs.uk/your-visit/patientinformation-leaflets/physiotherapy/
If you wish to consider some exercise, you may also find the resources on the following website helpful: www.nhs.uk/live-well/exercise
Advice regarding exercise in relation to pain problems can also be found at this previously mentioned resource, under ‘Improving Health & Fitness’.
There are sections on Tia chi, either in standing or seated, Stretches and Yoga.
For other videos contain advice and demonstration regarding Tai Chi exercises:
For videos containing advice and demonstration regards Pilates: https://www.nhs.uk/conditions/nhs-fitness-studio/?tabname=pilates-and-yoga
This includes pilates for MS & Fibromyalgia, Pilates for back pain, Pilates for arthritis and beginners pilates.
Information re Mental Health
Managing your pain can be difficult and at times, this will inevitably impact upon your Mental Health. The following are useful resources to support you with all aspects of your mental health.
https://www.mentalhealth.org.uk
There are currently free resources available on the ‘Headspace’ website and there is also an option to pay for annual subscription, should you choose, which allows you to access further resources. https://www.headspace.com/
https://www.torbayandsouthdevon.nhs.uk/services/healthy-lifestyles/improve-mood/
Associated Policies
Specialties
Places covered by
- vale-of-york
Hospital Trusts
- york-and-scarborough-teaching-hospitals